Construction and validation of a Nomogram model for assessing the risk of multidrug-resistant pulmonary tuberculosis infection in young people
-
摘要:
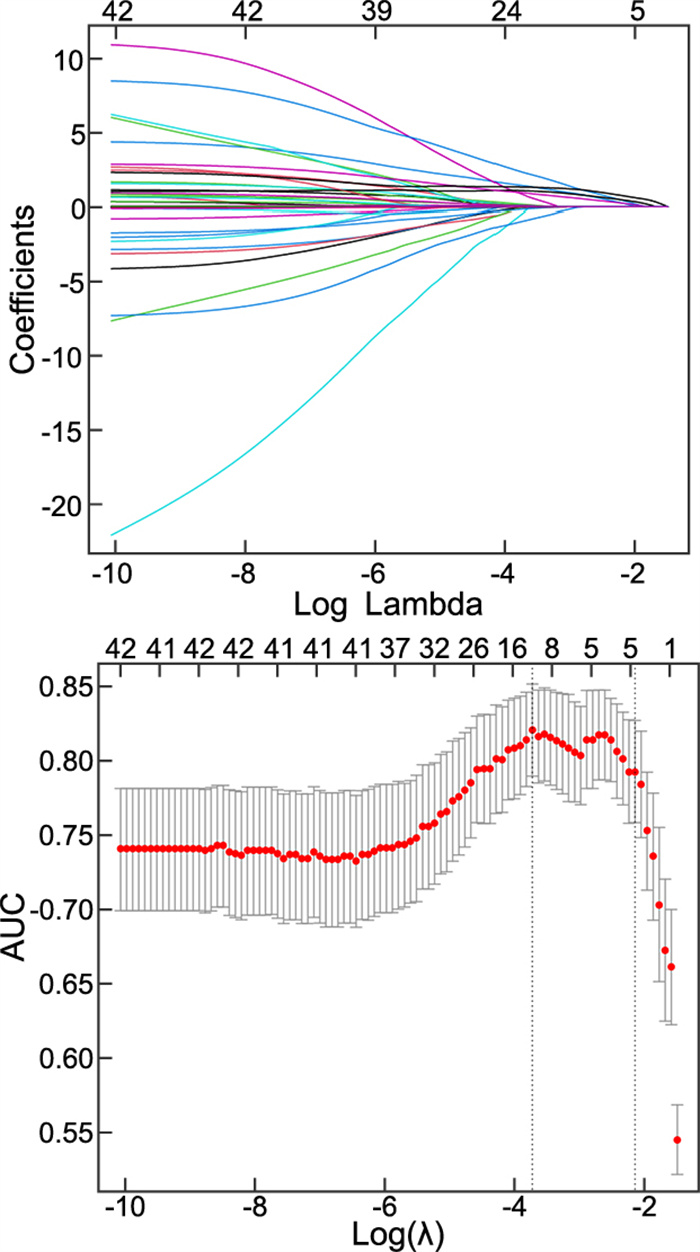
目的 探讨青年肺结核患者发生耐多药感染的危险因素, 构建风险列线图预测模型评估耐多药肺结核的发病风险。 方法 选择2019年1月—2021年12月安徽省胸科医院收治的明确诊断为肺结核的青年患者203例并收集临床资料。通过随机数字表法随机选择67例患者作为验证组, 另136例患者作为建模组, 根据是否发生耐药分为耐药组75例和非耐药组61例。通过Lasso回归和logistic回归分析研究青年肺结核患者发生耐药的危险因素, 构建Nomogram预测模型并进行验证。 结果 Logistic回归分析显示, 肺部空洞性病灶、营养不良、糖化血红蛋白高、痰涂片阳性、低收入是青年肺结核患者发生耐多药感染的独立危险因素。通过上述危险因素建立预测风险Nomogram模型, 建模组和验证组判断该模型的曲线下面积分别为0. 904、0. 743, 提示该模型有良好的诊断能力。Hosmer-Lemeshow检验结果提示建模组和验证组数据集中的曲线与模型拟合曲线差异无统计学意义, 表明该模型预测耐多药发生风险与实际感染风险的一致性较好, 拟合优度良好(P = 0. 438、0. 733)。 结论 基于Lasso回归和logistic回归分析建立的Nomogram模型预测能力强, 有助于评估青年肺结核患者发生耐多药感染的概率, 从而尽早做好干预措施, 改善患者预后。 Abstract:Objective This study aims to explore the risk factors for multidrug-resistant infections in young tuberculosis patients and construct a risk Nomogram model for assessing the incidence risk of multidrug-resistant tuberculosis. Methods From January 2019 to December 2021, 203 young patients with pulmonary tuberculosis were admitted to Anhui Chest Hospital, and their clinical data were collected. Using a random number table, the patients were divided into a validation group of 67 patients and a modeling group of 136 patients. Among them, there were 75 drug-resistant cases and 61 non-drug-resistant cases. Lasso regression and logistic regression were employed to analyze the risk factors for drug resistance in young pulmonary tuberculosis patients, following which a Nomogram prediction model was constructed and validated. Results Logistic regression analysis showed pulmonary cavitary lesions, innutrition, elevated glycosylated hemoglobin, positive sputum smear microscopy, and low income as independent risk factors for multidrug-resistant infection in young pulmonary tuberculosis patients. Using these risk factors, a Nomogram predictive model was constructed, with an area under the curve of 0. 904 for the modeling group and 0. 743 for the validation group, indicating good diagnostic accuracy. Hosmer-Lemeshow test results indicated no significant difference between the observed and model-predicted risks in both the modeling and validation datasets (P = 0. 438, 0. 733), suggesting good model fit and consistency with actual infection risks. Conclusion The Nomogram model, established using Lasso logistic regression analysis, exhibits high predictive capability for multidrug-resistant infection in young pulmonary tuberculosis patients. This enables prompt implementation of early intervention measures, ultimately improving prognosis. -
Key words:
- Drug resistant pulmonary tuberculosis /
- Risk factors /
- Prediction model /
- Nomogram
-
表 1 青年耐多药肺结核患者的多因素logistic回归分析
Table 1. Multivariate Logistic regression analysis of young people with MDR-TB
变量 B SE Waldχ2 P值 OR值 95% CI 低收入 2.167 0.570 14.467 < 0.001 8.731 2.858~26.668 营养不良 3.199 0.949 11.367 0.001 24.513 3.817~157.445 肺部空洞性病灶 1.639 0.512 10.247 0.001 5.151 1.888~14.055 痰涂片阳性 1.368 0.636 4.630 0.031 3.929 1.130~13.666 糖化血红蛋白高 2.053 0.707 8.443 0.004 7.790 1.951~31.112 -
[1] RANI C, PANDEY R K, UBAID-ULLAH S. Tuberculosis: an old enemy of mankind and possible next pandemic[M]. Emerging Pandemics. CRC Press, 2023: 47-62. [2] CHAKAYA J, KHAN M, NTOUMI F, et al. Global tuberculosis report 2020-reflections on the global TB burden, treatment and prevention efforts[J]. Int J Infect Dis, 2021, 113 Suppl 1(Suppl 1): S7-S12. [3] CHAKAYA J, PETERSEN E, NANTANDA R, et al. The WHO global tuberculosis 2021 report-not so good news and turning the tide back to end TB[J]. Int J Infect Dis, 2022, 124 Suppl 1: S26-S29. DOI: 10.1016/j.ijid.2022.03.011. [4] AKALU T Y, CLEMENTS A C, WOLDE H F, et al. Economic burden of multidrug-resistant tuberculosis on patients and households: a global systematic review and meta-analysis[J]. Sci Rep, 2023, 13(1): 22361. DOI: 10.1038/s41598-023-47094-9. [5] MIGLIORI G B, BEZOZZI G, GIRARDI E, et al. Clinical and operational value of the extensively drug-resistant tuberculosis definition[J]. Eur Respir J, 2007, 30(4): 623-626. [6] SANKINENI S, CHAUHAN S, SHEGOKAR R, et al. Global health and tuberculosis; past, present, and future[M]. Tubercular Drug Delivery Systems: Advances in Treatment of Infectious Diseases. Springer, 2023: 1-13. [7] 李伟. 耐多药肺结核患者心理健康与生活质量的影响因素分析[J]. 中国现代药物应用, 2023, 17(19): 13-17.LI W. Analysis of factors influencing mental health and quality of life in patients with multidrug-resistant tuberculosis[J]. Chinese Journal of Modern Drug Application, 2023, 17(19): 13-17. [8] 符婷, 黄丽菊, 杨进军, 等. 308例耐多药肺结核患者心理健康状况及其影响因素分析[J]. 中国防痨杂志, 2020, 42(4): 366-371.FU T, HUANG L J, YANG J J, et al. Psychological health status of 308 patients with MDR-PTB and its influencing factors[J]. Chinese Journal of Antituberculosis, 2020, 42(4): 366-371. [9] 邹级谦. 肺结核诊断标准[J]. 结核病健康教育, 2008(1): 7-9.ZOU J Q. Diagnostic criteria for pulmonary tuberculosis[J]. Tuberculosis Health Education, 2008(1): 7-9. [10] 卢春容, 房宏霞, 陆普选, 等. WHO 2021年全球结核病报告: 全球与中国关键数据分析[J]. 新发传染病电子杂志, 2021, 6(4): 368-372.LU C R, FANG H X, LU P X, et al. The global tuberculosis report 2021: key data analysis for China and the global world[J]. Electronic Journal of Emerging Infectious Diseases, 2021, 6(4): 368-372. [11] 徐彩红, 赵雁林. 从《2020年全球结核病报告》看我国结核病防治工作[J]. 中华传染病杂志, 2021, 39(7): 392-397.XU C H, ZHAO Y L. To evaluate the tuberculosis prevention and control situation in China from the perspective of global tuberculosis report 2020[J]. Chinese Journal of Infectious Diseases, 2021, 39(7): 392-397. [12] 王睿荣, 巨芳萍, 王娟, 等. 肺结核患者凝血功能和血小板计数变化及其临床意义[J]. 血栓与止血学, 2021, 27(2): 294-295.WANG R R, JU F P, WANG J, et al. Changes and Clinical Significance of Coagulation Function and Platelet Count in Patients with Pulmonary Tuberculosis[J]. Chinese Journal of Thrombosis and Hemostasis, 2021, 27(2): 294-295. [13] 郑珍慧, 江巧敏, 张尊敬. 基于倾向性评分法评估耐药肺结核患者疾病感知与服药依从性的相关性[J]. 中华全科医学, 2023, 21(11): 1872-1875. doi: 10.16766/j.cnki.issn.1674-4152.003246ZHENG Z H, JIANG Q M, ZHANG Z J. Evaluation of the association between disease perception and medication adherence in patients with drug-resistant pulmonary tuberculosis using the propensity score method[J]. Chinese Journal of General Practice, 2023, 21(11): 1872-1875. doi: 10.16766/j.cnki.issn.1674-4152.003246 [14] 刘慧梅, 张瑞梅, 刘加彬, 等. 1∶2个体匹配青年肺结核患者耐多药临床危险因素分析[J]. 山西医科大学学报, 2016, 47(9): 834-836.LIU H M, ZHANG R M, LIU J B, et al. A 1∶2 pair-matched study on risk factors of multi-drug resistance in young tuberculosis patients[J]. Journal of Shanxi Medical University, 2016, 47(9): 834-836. [15] WANG Y, CHUNG M J, SKRAHIN A, et al. Radiological signs associated with pulmonary multi-drug resistant tuberculosis: an analysis of published evidences[J]. Quant Imaging Med Surg, 2018, 8(2): 161-173. [16] CHENG N L, WU S, LUO X L, et al. A comparative study of chest computed tomography findings: 1 030 cases of drug-sensitive tuberculosis versus 516 cases of drug-resistant tuberculosis[J]. Infect Drug Resist, 2021, 14: 1115-1128. [17] RAJAMANICKAM A, MUNISANKAR S, DOLLA C K, et al. Undernutrition is associated with perturbations in T cell-, B cell-, monocyte-, and dendritic cell-subsets in latent Mycobacterium tuberculosis infection[J]. PLoS One, 2019, 14(12): e225611. DOI: 10.1371/journal.pone.0225611. [18] AYELIGN B, NEGASH M, GENETU M, et al. Immunological impacts of diabetes on the susceptibility of mycobacterium tuberculosis[J]. J Immunol Res, 2019, 2019(1): 6196532. DOI: 10.1155/2019/6196532. [19] 何启军, 姚敏, 吴秀继, 等. 免疫法测结核抗体与痰涂片镜检法的比较[J]. 中国热带医学, 2017, 17(4): 427-428.HE Q J, YAO M, WU X J, et al. Comparison of immune method and sputum smear microscopy method on anti-body tuberculosis[J]. China Tropical Medicine, 2017, 17(4): 427-428. -





 下载:
下载: