Prediction of traumatic coagulation disease based on the concept of hemorrhagic coagulation failure
-
摘要: 严重创伤救治是全球性难题,全球每年因严重创伤死亡人数约占总死亡数的10%,而创伤性凝血病(TIC)导致创伤性大出血占创伤患者死因的30%~40%。TIC由多因素与多系统所综合诱发,预防和纠正TIC是严重创伤或多发伤管理的核心之一,而复杂的发生机制致使其诊断标准滞后与救治不及时。有研究提出的出血性凝血衰竭理论认为:严重组织损伤和失血,导致休克低灌注与氧债的发生,同时伴随血管内皮的一系列病变反应启动了TIC的发生。本文基于这一机制理论,尝试建立能够预测TIC发生的综合指标组合。通过检索国内外相关文献,综述了在血性凝血衰竭过程中的重要临床指标变化,以及这些指标对TIC的发生与进展的影响。创伤严重程度评分,代表出血休克的血红蛋白变化、平均动脉压和休克指数,反映低灌注与无氧代谢的乳酸、pH值与碱剩余指标,血管内皮糖萼、syndecan-1、血管内皮细胞标记物血栓调节蛋白(TM)与血管性血友病因子(VWF)因子等指标均具有评估患者TIC发生发展的潜在价值。因此,从出血性凝血衰竭发生机制的角度出发,了解由严重组织创伤、创伤性休克和组织低灌注,继而导致的血管内皮病变过程所诱导的TIC发生机制,能够为实施TIC的早期诊断乃至救治提供可靠的指标组合。Abstract: The treatment of severe trauma is a global problem. The deaths due to severe trauma accounts for about 10% of the total deaths every year, and the traumatic hemorrhage that caused by trauma-induced coagulopathy (TIC) accounts for 30%-40% of deaths in trauma patients. TIC is comprehensively induced by multiple factors and systems, and the prevention and treatment of TIC is one of the cores of the management of severe trauma or multiple injuries. The complicated mechanism makes the diagnosis and treatment of TIC not timely. The hemorrhagic coagulation failure believes that sever tissue damage and blood loss lead to shock hypoperfusion and oxygen debt, and a series of pathological reactions of the vascular endothelium initiates the occurrence of TIC. This paper attempts to establish a combination of indicators to predict the occurrence of TIC on the basis of this theory. By selecting relevant domestic and foreign literature, the important clinical indicators that involved in the process of blood coagulation failure and the impact of them on the occurrence and progress of TIC were reviewed. The injury severity score, hemoglobin changes, mean arterial pressure, shock index, lactic acid, pH, alkali excess, vascular endothelial glycocalyx, syndecan-1, thrombomodulin (TM) and von Willebrand factor(VWF) factors all have the potential value of evaluating the occurrence and development of TIC in patients. From the perspective of the mechanism of hemorrhagic coagulation failure understanding the mechanism of TIC followed severe tissue trauma, traumatic shock and tissue hypoperfusion and the vascular endothelial disease subsequently, can be used for the implementation of early diagnosis and even treatment of TIC, and also provide reliable combined indicators.
-
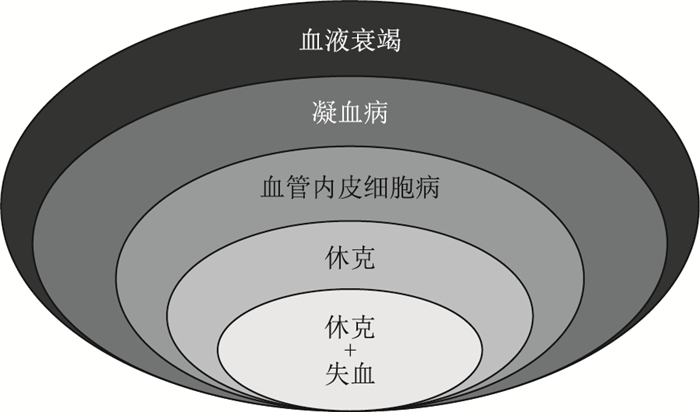
图 1 出血性血液衰竭启动和进展示意图
注:严重组织损伤和失血,休克低灌注、氧债发生,在伴随炎症反应和交感肾上腺素激活作用下血管内皮脱落,内皮细胞暴露,血管内皮病发生,启动凝血,最终导致凝血因子活性降低、纤溶亢进和血小板功能障碍,引发出血性血液衰竭。图片来源于文献[14]。
Figure 1. Schematic diagram of initiation and progression of hemorrhagic blood failure
-
[1] GBD 2016 CAUSES OF DEATH COLLABORATORS. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016 a systematic analysis for the Global Burden of Disease Study 2016[J]. Lancet, 2017, 390(10100): 1151-1210. doi: 10.1016/S0140-6736(17)32152-9 [2] ZHANG J, ZHANG F, DONG J F. Coagulopathy induced by traumatic brain injury: Systemic manifestation of a localized injury[J]. Blood, 2018, 131(18): 2001-2006. doi: 10.1182/blood-2017-11-784108 [3] SPAHN D R, BOUILLON B, CERNY V, et al. The European guideline on management of major bleeding and coagulopathy following trauma: Fifth edition[J]. Crit Care, 2019, 23(1): 98. doi: 10.1186/s13054-019-2347-3 [4] KORNBLITH L Z, MOORE H B, COHEN M J. Tramua-induced coagulopathy: The past, present, and future[J]. J Thromb Haemost, 2019, 17(6): 852-862. doi: 10.1111/jth.14450 [5] CHANG R, CARDENAS J C, WADE C E, et al. Advances in the understanding of trauma-induced coagulopathy[J]. Blood, 2016, 128(8): 1043-1049. doi: 10.1182/blood-2016-01-636423 [6] BOHM J K, SCHAFER N, MAEGELE M, et al. Plasmatic and cell-based enhancement by microparticles originated from platelets and endothelial cells under simulated in vitro conditions of a dilutional coagulopathy[J]. Scand J Trauma Resusc Emerg Med, 2021, 29(1): 38. doi: 10.1186/s13049-021-00847-9 [7] CASPERS M, MAEGELE M, FROHLICH M. Current strategies for hemostatic control in acute trauma hemorrhage and trauma-induced coagulopathy[J]. Expert Rev Hematol, 2018, 11(12): 987-995. doi: 10.1080/17474086.2018.1548929 [8] NATHAN J W, KEVIN R W, PATI S, et al. Hemorrhagic blood failure: Oxygen debt, coagulopathy, and endothelial damage[J]. J Trauma Acute Care Surg, 2017, 82(6S): S41-S49. doi: 10.1097/TA.0000000000001436 [9] 田勇, 卜瑞红, 解彦格, 等. 乌司他丁对创伤性凝血病患者凝血功能及炎症因子的影响[J]. 中国临床研究, 2018, 31(3): 369-372. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGCK201803020.htmTIAN Y, BU R H, XIE Y G, et al. Effect of ulinastatin on coagulation function and inflammatory cytokines in patients with traumatic coagulation disease[J]. Chinese Journal of Clinical Research, 2018, 31(3): 369-372. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGCK201803020.htm [10] 张志华, 余国峰. 血栓弹力图用于诊断颅脑损伤后创伤性凝血病的临床研究[J]. 中华全科医学, 2021, 19(8): 1300-1302, 1329. doi: 10.16766/j.cnki.issn.1674-4152.002045ZHANG Z H, YU G F. Clinical study of thromboelastography in the diagnosis of traumatic coagulopathy after craniocerebral injury[J]. Chinese Journal of General Practice, 2021, 19(8): 1300-1302, 1329. doi: 10.16766/j.cnki.issn.1674-4152.002045 [11] CHOW J H, RICHARDS J E, MORRISON J J, et al. Viscoelastic signals for optimal resuscitation in trauma: Kaolin thrombelastography cutoffs for diagnosing hypofibrinogenemia (VISOR Study)[J]. Anesth Analg, 2019, 129(6): 1482-1491. doi: 10.1213/ANE.0000000000004315 [12] GEOFFREY P D, JODIE L M, LISA M D, et al. Traumatic-induced coagulopathy as a systems failure: A new window into hemostasis[J]. Semin Thromb Hemost, 2020, 46(2): 199-214. doi: 10.1055/s-0039-1701018 [13] TRANCA S, PETRISOR C, HAGAU N, et al. Can APACHE Ⅱ, SOFA, ISS, and RTS severity scores be used to predict septic complications in multiple trauma patients[J]. J Crit Care Med, 2016, 2(3): 124-130. doi: 10.1515/jccm-2016-0019 [14] NEEKI M M, DONG F, TOY J, et al. Safety and efficacy of hospital utilization of tranexamic acid in civilian adult trauma resuscitation[J]. West J Emerg Med, 2020, 21(2): 217-225. doi: 10.5811/westjem.2019.10.43055 [15] DEYNSE H V, COOLS W, DEPREITERE B, et al. Quantifying injury severity for traumatic brain injury with routinely collected health data[J]. Injury, 2022, 53(1): 11-20. doi: 10.1016/j.injury.2021.10.013 [16] CARIUS P H, HOFMANN G O, LEFERING R, et al. Clinical presentation and blood gas analysis of multiple trauma patients for prediction of standard coagulation parameters at emergency department arrival[J]. Anaesthesist, 2016, 65(4): 274-280. doi: 10.1007/s00101-016-0150-y [17] 沈哲源, 田书委, 孔宇, 等. 创伤性凝血病发病机制及诊治研究进展[J]. 中华创伤杂志, 2018, 34(4): 377-384. doi: 10.3760/cma.j.issn.1001-8050.2018.04.015SHEN Z Y, TIAN S W, KONG Y, et al. Research advances in pathophysiology, diagnosis and therapy of trauma-induced coagulopathy[J]. Chinese Journal of Traumatology, 2018, 34(4): 377-384. doi: 10.3760/cma.j.issn.1001-8050.2018.04.015 [18] AN Z P, HUANG H B, WANG Z G, et al. Correlation between plasma D-Dimer level and severity and prognosis in patients admitted at emergency department with trauma[J]. Clin Lab, 2020, 66(1). DOI: 10.7754/Clin.Lab.2019.190520. [19] BJERKVIG C K, STRANDENES G, ELIASSEN H S, et al. "Blood failure" time to view blood as an organ: How oxygen debt contributes to blood failure and its implications for remote damage control resuscitation[J]. Transfusion, 2016, 56(Suppl 2): S182-S189. [20] HAYAKAWA M, MAEKAWA K, KUSHIMOTO S, et al. High-dimer levels predicate a poor outcome in patients with severe trauma, even with high fibrinogen levels on arrival: A multicenter retrospective study[J]. Shock, 2016, 45(3): 308-314. doi: 10.1097/SHK.0000000000000542 [21] 田勇, 卜瑞红, 解彦格, 等. 急性创伤性凝血病不同预后患者外周血APC、vWF、D-D水平变化及意义[J]. 山东医药, 2017, 57(34): 75-77. doi: 10.3969/j.issn.1002-266X.2017.34.025TIAN Y, BU R H, XIE Y G, et al. Changes of peripheral blood APC, vWF and D-D in patients with acute traumatic coagulopathy with different prognoses and their significance[J]. Shandong Medical Journal, 2017, 57(34): 75-77. doi: 10.3969/j.issn.1002-266X.2017.34.025 [22] NAKAE R, FUJIKI Y, TAKAYAMA Y, et al. Age-related differences in the time course of coagulation and fibrinolytic parameters in patients with traumatic brain injury[J]. Int J Mol Sci, 2020, 21(16): 5613. doi: 10.3390/ijms21165613 [23] SETH D, HAUSLADEN A, STAMLER J S. Anaerobic transcription by OxyR: A novel paradigm for nitrosative stress[J]. Antioxid Redox Signal, 2020, 32(12): 803-816. doi: 10.1089/ars.2019.7921 [24] THOMAS M, BENOV L. The contribution of superoxide radical to cadmium toxicity in E. coli[J]. Biol Trace Elem Res, 2018, 181(2): 361-368. doi: 10.1007/s12011-017-1048-5 [25] RABINOWITZ J D, ENERBACK S. Lactate: The ugly duckling of energy metabolism[J]. Nat Metab, 2020, 2(7): 566-571. doi: 10.1038/s42255-020-0243-4 [26] 张丽英, 肖毅, 张红, 等. 乳酸清除率、C反应蛋白和CURB-65评分在评估急诊重症肺炎预后中的作用[J]. 北京医学, 2021, 43(5): 460-462, 465. https://www.cnki.com.cn/Article/CJFDTOTAL-BJYX202105025.htmZHANG L Y, XIAO Y, ZHANG H, et al. The role of lactate clearance, C-reactive protein and CURB-65 score in evaluating the prognosis of acute severe pneumonia[J]. Beijing Medical Journal, 2021, 43(5): 460-462, 465. https://www.cnki.com.cn/Article/CJFDTOTAL-BJYX202105025.htm [27] JOFFRE J, HELLMAN J, INCE C, et al. Endothelial responses in sepsis[J]. Am J Respir Crit Care Med, 2020, 202(3): 361-370. doi: 10.1164/rccm.201910-1911TR [28] GODO S, SHIMOKAWA H. Endothelial functions[J]. Arterioscler Thromb Vasc Biol, 2017, 37(9): e108-e114. [29] UCHIDA K, NISHIMURA T, HAGAWA N, et al. The impact of early administration of vasopressor agents for the resuscitation of severe hemorrhagic shock following blunt trauma[J]. BMC Emerg Med, 2020, 20(1): 26. doi: 10.1186/s12873-020-00322-1 [30] CASH A, THEUS M H. Mechanisms of blood-brain barrier dysfunction in traumatic brain injury[J]. Int J Mol Sci, 2020, 21(9): 3344. doi: 10.3390/ijms21093344 [31] JOHANSSON P I, HENRIKSEN H H, STENSBALLE J, et al. Traumatic endotheliopathy: A prospective observational study of 424 severely injured patients[J]. Ann Surg, 2017, 265(3): 597-603. doi: 10.1097/SLA.0000000000001751 [32] PILLINGER N L, KAM P. Endothelial glycocalyx: Basic science and clinical implications[J]. Anaesth Intensive Care, 2017, 45(3): 295-307. doi: 10.1177/0310057X1704500305 [33] CAHILL P A, REDMOND E M. Vascular endothelium: Gatekeeper of vessel health[J]. Atherosclerosis, 2016, 248: 97-109. doi: 10.1016/j.atherosclerosis.2016.03.007 [34] ABASSI Z, ARMALY Z, HEYMAN S N. Glycocalyx degradation in ischemia-reperfusion injury[J]. Am J Pathol, 2020, 190(4): 752-767. doi: 10.1016/j.ajpath.2019.08.019 [35] DESIDERI S, ONIONS K L, BAKER S L, et al. Endothelial glycocalyx restoration by growth factors in diabetic nephropathy[J]. Biorheology, 2019, 56(2-3): 163-179. doi: 10.3233/BIR-180199 [36] COSGUN Z C, FELS B, VIHROG K K. Nanomechanics of the endothelial glycocalyx: From structure to function[J]. Am J Pathol, 2020, 190(4): 732-741. doi: 10.1016/j.ajpath.2019.07.021 [37] ABDULLAH S, KARIM M, LEGENDRE M, et al. Hemorrhagic shock and resuscitation causes glycocalyx shedding and endothelial oxidative stress preferentially in the lung and intestinal vasculature[J]. Shock, 2021, 56(5): 803-812. doi: 10.1097/SHK.0000000000001764 [38] CHIPMAN A M, WU F, KOZAR R A. Fibrinogen inhibits microRNA-19b, a novel mechanism for repair of haemorrhagic shock-induced endothelial cell dysfunction[J]. Blood Transfus, 2021, 19(5): 420-427. [39] MISHRA A K, DINGLI D. Metformin inhibits IL-6 signaling by decreasing IL-6R expression on multiple myeloma cells[J]. Leukemia, 2019, 33(11): 2695-2709. doi: 10.1038/s41375-019-0470-4 [40] DUQUE P, MORA L, LEVY J H. et al. Pathophysiological response to trauma-induced coagulopathy: A comprehensive review[J]. Anesth Analg, 2020, 130(3): 654-664. doi: 10.1213/ANE.0000000000004478 [41] PETROS S. Trauma-induced coagulopathy[J]. Hamostaseologie, 2019, 39(1): 20-27. doi: 10.1055/s-0039-1677853 [42] MINSKY B B, ABZALIMOV R R, NIU C, et al. Mass spectrometry revels a multifaceted role of glycosaminoglycan chains in factor Xa inactivation by antithrombin[J]. Biochemistry, 2018, 57(32): 4880-4890. [43] CHANG R, CARDENAS J C, WADE C E, et al. Advances in the understanding of trauma-induced coagulopathy[J]. Blood, 2016, 128(8): 1043-1049. doi: 10.1182/blood-2016-01-636423 [44] NAKANO T, TAKAHASHI T, YAMAMOTO C, et al. Arsenite inhibits tissue-type plasminogen activator synthesis through NRF2 activation in cultured human vascular endothelial EA. hy926 cells[J]. Int J Mol Sci, 2021, 22(2): 739. [45] ANDRIANTO A, AL-FARABI M J, NUGRAHA R A, et al. Biomarkers of endothelial dysfunction and outcomes in coronavirus disease 2019 (COVID-19) patients: A systematic review and meta-analysis[J]. Mircovasc Res, 2021, 138: 104224. [46] SALEH J, PEYSSONNAUX C, SINGH K K, et al. Mitochondria and microbiota dysfunction in COVID-19 pathogenesis[J]. Mitochondrion, 2020, 54(4): 1-7. [47] WU S C, RAU C S, KUO S C H, et al. Shock index increase from the field to the emergency room is associate with higher odds of massive transfusion in trauma patients with stable blood pressure: A cross-sectional analysis[J]. Am Surg, 2019, 14(4): e0216153. [48] ODOM S R, HOWELL M D, GUPTA A, et al. Extremes of shock index predicts death in trauma patients[J]. J Emerg Trauma Shock, 2016, 9(3): 103-106. [49] DE LUCAS E H, SANCHEZ M S, FUCINOS L C, et al. Lactate and lactate clearance in critically burned patients: Usefulness and limitations as a resuscitation guide and as a prognostic factor[J]. Burns, 2020, 46(8): 1839-1847. [50] RAHBAR E, CARDENAS J C, BAIMUKANOVA G, et al. Endothelial glycocalyx shedding and vascular permeability in severely injured trauma patients[J]. J Transl Med, 2015;13: 117. -





 下载:
下载: