Risk factors for adjacent segment refracture after percutaneous kyphoplasty
-
摘要:
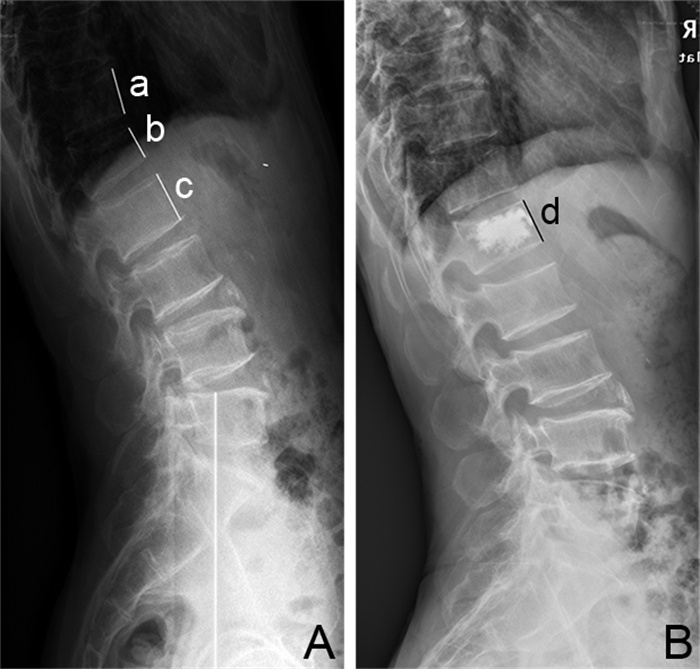
目的 对经皮椎体后凸成形术(PKP)术后邻近椎体再骨折的相关危险因素进行分析和探讨, 以减少骨质疏松性椎体压缩性骨折(OVCF)术后邻近节段再骨折的发生。 方法 收集2016年1月—2017年12月浙江中医药大学附属第二医院骨科行PKP术治疗的438例单节段OVCF患者的资料进行回顾性分析。依据PKP术后是否发生邻近节段再骨折分为再骨折组(32例)和非骨折组(257例)。比较2组患者的年龄、性别、体重指数、胸腰段比例、骨密度、骨水泥注入量、椎体高度恢复率、骨水泥渗漏情况、随访期间外伤情况及再骨折时骨密度,对这些因素进行单因素分析,将其中差异有统计学意义的因素纳入多因素logistic回归模型中,分析其与邻近节段再骨折的相关性。 结果 289例患者随访资料完整并纳入本研究,术后随访12~24(13.5±0.9)个月。至末次随访,术后共32例患者新发生邻近椎体骨折。单因素分析结果显示,邻近节段再骨折与再骨折时骨密度和随访期间外伤情况有关(均P<0.05)。多因素logistic回归分析结果显示,再骨折时骨密度(OR=0.225)是术后邻近节段再骨折的影响因素(P < 0.01);随访期间轻微外伤(OR=5.254)可能是导致再骨折发生的重要外部影响因素(P < 0.01)。 结论 PKP术后邻近节段再骨折的发生主要原因是骨质疏松的进展和随访期间的再次外伤。因此术后早期腰围保护和正规抗骨质疏松治疗及避免外伤必不可少。 -
关键词:
- 骨质疏松性骨折 /
- 经皮椎体后凸成形术 /
- 再骨折 /
- 危险因素 /
- Logistic回归分析
Abstract:Objective To analyze the risk factors for adjacent segment refracture after percutaneous kyphoplasty (PKP), so as to reduce the incidence of adjacent segmental refracture in patients with osteoporotic vertebral compression fracture (OVCF) after PKP. Methods Total 438 patients with single-segment OVCF treated by PKP in the Department of Orthopedics of the Second Affiliated Hospital of Zhejiang University of Traditional Chinese Medicine from January 2016 to December 2017 were collected and analyzed retrospectively. The patients were divided into refracture group (32 cases) and non-fracture group (257 cases) according to the occurrence of adjacent segment fracture after PKP. The age, gender, body mass index (BMI), proportion of injured vertebrae in thoracolumbar segment, bone mineral density, bone cement injection volume, recovery rate of vertebral height, bone cement leakage, trauma during follow-up and bone mineral density during refracture in the two groups were analyzed by univariate analysis. The statistically significant factors were put into logistic regression to analyze their correlation with adjacent segment refractures after PKP. Results The follow-up data of 289 patients were complete and included in this study, the postoperative follow-up was 12 to 24 (13.5±0.9) months. Up to the last follow-up, 32 patients had new adjacent vertebral fractures. Univariate analysis showed that the refracture of adjacent segments was correlated with bone mineral density at the time of refracture and trauma during follow-up (P < 0.05). Multivariate logistic regression analysis showed that the bone mineral density at the time of refracture (OR=0.225) was the influencing factor of postoperative adjacent segment refracture (P < 0.01). Minor trauma during follow-up (OR=5.254) might be an important external factor leading to the occurrence of adjacent segment refracture (P < 0.01). Conclusion The main causes of adjacent segment refracture after PKP are severe osteoporosis and trauma during follow-up. Therefore, early postoperative waist protection, effective anti-osteoporosis treatment and avoidance of trauma are essential. -
表 1 PKP后NVCF的单因素分析
Table 1. Single-factor analysis of New Vertebral Compression Fracture after percutaneous kyphoplasty
项目 再骨折组(32例) 非骨折组(257例) 统计量 P值 性别(例) 0.175a 0.675 男性 11 79 女性 21 178 年龄(x±s,岁) 70.25±9.15 71.69±10.34 0.753b 0.452 治疗前骨密度T值(x±s) -2.76±0.49 -2.87±0.61 -1.179b 0.245 初次骨折伤椎区域(例) 1.868a 0.172 胸腰椎区 21 197 非胸腰椎区 11 60 BMI(x±s) 23.68±4.87 24.25±5.09 -0.624b 0.533 伤椎高度恢复率(x±s,%) 56.88±28.10 54.19±25.35 -0.559b 0.577 骨水泥渗漏情况(例) 3.047a 0.081 有 12 60 无 20 197 骨水泥注入量(x±s,mL) 4.04±1.91 3.93±1.76 -0.311b 0.756 再骨折时/末次随访时骨密度T值(x±s) -3.37±0.40 -3.02±0.55 4.384b <0.001 随访期间外伤情况(例) 16.119a <0.001 有 15 43 无 17 214 注:a为χ2值,b为t值。 表 2 术后再发椎体骨折相关因素的logistic回归分析
Table 2. Logistic regression analysis of related factors of postoperative recurrent vertebral fracture
变量 B SE Wald χ2 P值 OR值 95% CI 骨密度 -1.492 0.426 12.241 <0.001 0.225 0.098~0.519 随访期间外伤 1.659 0.415 15.971 <0.001 5.254 2.329~11.853 -
[1] WANG B, ZHAO C P, SONG L X, et al. Balloon kyphoplasty versus percutaneous vertebroplasty for osteoporotic vertebral compression fracture: A meta-analysis and systematic review[J]. J Orthop Surg Res, 2018, 13(1): 264. doi: 10.1186/s13018-018-0952-5 [2] PARREIRA P C S, MACHER C G, MEGALE R Z, et al. An overview of clinical guidelines for the management of vertebral compression fracture: A systematic review[J]. Spine J, 2017, 17(12): 1932-1938. doi: 10.1016/j.spinee.2017.07.174 [3] SANLI I, KUIJK S M J, BIE R A D, et al. Percutaneous cement augmentation in the treatment of osteoporotic vertebral fractures (OVFs) in the elderly: A systematic review[J]. Eur Spine J, 2020, 29(7): 1553-1572. doi: 10.1007/s00586-020-06391-x [4] YU W B, XU W X, JIANG X B, et al. Risk factors for recollapse of the augmented vertebrae after percutaneous vertebral augmentation: A systematic review and meta-analysis[J]. World Neurosurg, 2018, 111(3): 119-129. [5] 韩晓东, 孟纯阳. PVP术后椎体前缘高度恢复率与邻近椎体骨折的相关性研究[J]. 中国矫形外科杂志, 2019, 27(10): 885-889. https://www.cnki.com.cn/Article/CJFDTOTAL-ZJXS201910007.htmHAN CD, MENG CY. Correlation between anterior vertebral height recovery rate and new-onset adjacent vertebral body fracture after percutaneous vertebroplasty[J]. Orthopedic Journal of China, 2019, 27(10): 885-889. https://www.cnki.com.cn/Article/CJFDTOTAL-ZJXS201910007.htm [6] ZHANG H, XU C Y, ZHANG T X, et al. Does percutaneous vertebroplasty or balloon kyphoplasty for osteoporotic vertebral compression fractures increase the incidence of new vertebral fractures? A meta-analysis[J]. Pain Physician, 2017, 20(1): E13-E28. [7] CAMACHO P M, PETAK S M, BINKLEY N, et al. American association of clinical endocrinologists/American college of endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis-2020 update[J]. Endocr Pract, 2020, 26(5): 564-570. doi: 10.4158/GL-2020-0524 [8] 田野, 郑博隆, 陈浩, 等. 骨质疏松性胸腰椎骨折治疗的研究进展[J]. 骨科, 2019, 10(5): 480-484. doi: 10.3969/j.issn.1674-8573.2019.05.023TIAN Y, ZHENG BL, CHEN H. Research progress in the treatment of osteoporotic thoracolumbar fractures[J]. Orthopaedics, 2019, 10(5): 480-484. doi: 10.3969/j.issn.1674-8573.2019.05.023 [9] 唐杰, 臧传义, 王健. 单侧与双侧经皮椎体后凸成形术治疗老年骨质疏松压缩性骨折的疗效及安全性比较[J]. 北京医学, 2020, 42(2): 113-116. https://www.cnki.com.cn/Article/CJFDTOTAL-BJYX202002006.htmTANG J, ZANG CY, WANG J. Comparison of efficacy and safety of unilateral and bilateral percutaneous kyphoplasty in the treatment of senile osteoporotic compression fractures[J]. Beijing Medical Journal, 2020, 42(02): 113-116. https://www.cnki.com.cn/Article/CJFDTOTAL-BJYX202002006.htm [10] LEE B G, CHOI J H, KIM D Y, et al. Risk factors for newly developed osteoporotic vertebral compression fractures following treatment for osteoporotic vertebral compression fractures[J]. Spine J, 2019, 19(2): 301-305. doi: 10.1016/j.spinee.2018.06.347 [11] 吴健, 关月红, 范胜利. 单节段胸腰段骨折经皮后凸成形术后再骨折的风险因素分析[J]. 中国骨伤, 2017, 30(9): 833-837. doi: 10.3969/j.issn.1003-0034.2017.09.010WU J, GUAN YH, FAN SL. Risk factors of non surgical vertebral fracture after percutaneous kyphoplasty of single segment thoracolumbar fracture[J]. China Journal of Orthopaedics and Traumatology, 2017, 30(9): 833-837. doi: 10.3969/j.issn.1003-0034.2017.09.010 [12] HE S J, ZHANG Y J, LV N N, et al. The effect of bone cement distribution on clinical efficacy after percutaneous kyphoplasty for osteoporotic vertebral compression fractures[J]. Medicine, 2019, 98(50): e18217. DOI: 10.1097/MD.0000000000018217. [13] BAE J S, PARK J H, KIM K J, et al. Analysis of risk factors for secondary new vertebral compression fracture following percutaneous vertebroplasty in patients with osteoporosis[J]. World Neurosurg, 2017, 99(3): 387-394. [14] BORENSZTEIN M, CAMINO WILLHUBER G O, POSADAS MARTINEZ M L, et al. Analysis of risk factors for new vertebral fracture after percutaneous vertebroplasty[J]. Global Spine J, 2018, 8(5): 446-452. doi: 10.1177/2192568217732988 [15] LI Y X, GUO D Q, ZHANG S C. Risk factor analysis for re-collapse of cemented vertebrae after percutaneous vertebroplasty (PVP) or percutaneous kyphoplasty (PKP)[J]. Int Orthop, 2018, 42(9): 2131-2139. doi: 10.1007/s00264-018-3838-6 [16] MOONEY J H, AMBURGY J, SELF M, et al. Vertebral height restoration following kyphoplasty[J]. J Spine Surg, 2019, 5(2): 194-200. doi: 10.21037/jss.2019.04.02 [17] SUN H B, JING X S, TANG H, et al. Clinical and radiological subsequent fractures after vertebral augmentation for treating osteoporotic vertebral compression fractures: A meta-analysis[J]. Eur Spine J, 2020, 29(10): 2576-2590. doi: 10.1007/s00586-020-06560-y [18] 何丽蔚, 徐煜, 颜程, 等. 老年人骨质疏松性骨折风险与脊柱活动能力及脊柱曲度的关系[J]. 中华全科医学, 2017, 15(4): 687-689, 723. doi: 10.16766/j.cnki.issn.1674-4152.2017.04.043HE LW, XU Y, YAN C, et al. The relationship between the risk of osteoporotic fracture and spine activity and spine curvature in the elderly[J]. Chinese Journal of General Practice, 2017, 15(4): 687-689, 723. doi: 10.16766/j.cnki.issn.1674-4152.2017.04.043 [19] YANG W C, YANG J Y, LIANG M. Percutaneous vertebroplasty does not increase the incidence of new fractures in adjacent and nonadjacent vertebral bodies[J]. Clin Spine Surg, 2019, 32(2): E99-E106. doi: 10.1097/BSD.0000000000000734 [20] YANG W C, SONG J T, LIANG M, et al. Functional outcomes and new vertebral fractures in percutaneous vertebroplasty and conservative treatment of acute symptomatic osteoporotic vertebral compression fractures[J]. World Neurosurg, 2019, 131(10): e346-e352. -





 下载:
下载: