Prediction of prognosis in elderly nHCM patients using nomogram based on CMR and clinical characteristics
-
摘要:
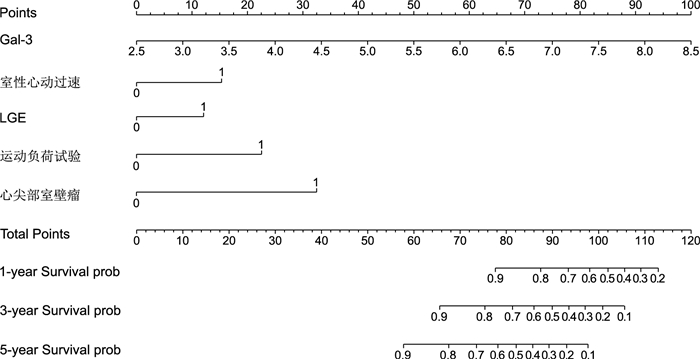
目的 探讨老年非梗阻性肥厚型心肌病(nHCM)患者的生存预后,并建立一个基于心脏核磁共振(CMR)参数与临床特征的诺莫图来个体化评估nHCM患者的预后。 方法 回顾性分析2015年6月—2021年11月于遂宁市中心医院心血管中心与南充市中心医院心内科住院的179例nHCM患者,采用多因素Cox回归分析确定与患者OS相关的独立预后因素并绘制诺莫图,采用重采样法(Bootstrap)进行评估验证。 结果 多因素Cox回归分析显示影响预后的因素为半乳糖凝集素-3(Gal-3)、室性心动过速、心尖部室壁瘤、延迟强化(LGE)、运动负荷试验。基于以上因素绘制诺莫图,一致性指数(C-index)的Bootstrap校正值为0.908(95% CI:0.869~0.947)。区分度分析采用多时点ROC曲线计算1、3、5年生存率曲线下面积为0.907、0.935、0.921。校准曲线显示预测估计风险与实际观测结果有较好的准确度。 结论 Gal-3升高、室性心动过速、心尖部室壁瘤、运动负荷试验阳性与基于CMR参数中的LGE阳性是影响老年nHCM患者预后的独立危险因素;结合上述指标构建的诺莫图可以个体化评估老年nHCM患者的预后。 -
关键词:
- 非梗阻性肥厚型心肌病 /
- 心脏磁共振 /
- 诺莫图 /
- 预后
Abstract:Objective To investigate the survival prognosis of elderly patients with non-obstructive hypertrophic cardiomyopathy (nHCM), and to establish a nomogram based on cardiac magnetic resonance (CMR) parameters and clinical characteristics to predict the overall survival (OS) of patients with nHCM. Methods A total of 179 patients with nHCM admitted to the Cardiovascular Center of Suining Central Hospital and Nanchong Central Hospital from June 2015 to November 2021 were retrospectively analyzed. Multivariate Cox regression analysis was used to determine the independent prognostic factors associated with OS and nomogram was drawn. The internal validation was performed by Bootstrap. Results Multivariate Cox regression analysis showed that the prognostic factors were galectin-3 (Gal-3), ventricular tachycardia, apical aneurysm, late gadolinium enhancement (LGE), exercise stress test. The Bootstrap correction value of c-index was 0.908(95% CI: 0.869-0.947); The area under the curve of 1, 3, and 5-year survival rate calculated by multi time point ROC curve were 0.907, 0.935, and 0.921 for discrimination analysis. The calibration curve showed that the predicted estimated risk had good accuracy with the actual observation results. Conclusion The elevation of Gal-3, ventricular tachycardia, apical ventricular aneurysm, positive exercise stress test, and positive LGE based on CMR parameters are independent risk factors that affect the prognosis of elderly nHCM patients. The nomogram constructed based on the above indicators can be used to individualize the assessment of the prognosis of elderly nHCM patients. -
表 1 事件组与非事件组基线资料比较
Table 1. Comparison of baseline data between the event group and non-event group
项目 非事件组(n=149) 事件组(n=30) 统计量 P值 年龄(x±s,岁) 70.1±6.9 69.9±6.1 0.166a 0.917 性别(男性/女性,例) 87/62 15/15 0.416b 0.519 猝死家族史[例(%)] 47(31.5) 11(36.7) 0.111b 0.739 冠心病[例(%)] 43(28.9) 10(33.3) 0.073b 0.787 慢性肾脏病[例(%)] 28(18.8) 4(13.3) 0.203b 0.652 缺血性脑卒中[例(%)] 26(17.4) 4(13.3) 0.080b 0.777 房颤/房扑[例(%)] 36(24.2) 7(23.3) 0.019b 0.999 室性心动过速[例(%)] 24(16.1) 15(50.0) 14.903b < 0.001 晕厥或先兆晕厥[例(%)] 17(11.4) 10(33.3) 0.545b 0.005 脑利钠肽前体[M(P25, P75), ng/L] 534(417, 697) 604(408, 979) 0.455c 0.122 超敏肌钙蛋白[M(P25, P75), μg/L] 0.73(0.56, 0.92) 0.84(0.66, 1.08) 0.173c 0.399 Gal-3[M(P25, P75), μg/L] 4.32(3.72, 4.80) 6.26(5.47, 6.65) 2.118c < 0.001 血尿素氮(x±s, mmol/L) 5.71±2.36 6.72±4.04 1.325a 0.194 运动负荷试验阳性[例(%)] 12(8.1) 9(30.0) 0.582b 0.002 肺动脉压升高[例(%)] 38(25.5) 8(26.7) 0.026b 0.999 QTc间期[M(P25, P75), ms] 435(410, 473) 463(441, 493) 3.947c 0.010 Tp-Te间期(x±s,ms) 102.0±18.1 99.4±13.3 0.892a 0.377 LVEF(x±s,%) 53.7±8.4 47.9±3.8 5.942a < 0.001 LAEDD[M(P25, P75), mm] 33.0(29.0, 39.0) 34.0(29.2, 40.4) 0.122c 0.496 RAEDD[M(P25, P75), mm] 42.0(40.0, 43.0) 42.0(40.0, 44.8) 0.795c 0.421 LVEDD(x±s,mm) 46.4±4.2 46.0±3.1 0.651a 0.518 RVEDD[M(P25, P75), mm] 26.0(24.0, 28.0) 25.0(24.0, 27.0) 0.918c 0.300 EDV(x±s,mL/m2) 147.0±22.8 151.0±22.4 0.858a 0.396 ESV(x±s,mL/m2) 48.9±19.2 55.7±18.4 1.829a 0.074 SV(x±s,mL/m2) 107.0±15.6 108.0±15.4 0.423a 0.674 CO[M(P25, P75), L/min] 2.8(2.5, 3.4) 2.9(2.5, 3.4) 0.084c 0.685 CI(x±s,L/min·m2) 2.9±0.7 2.9±0.7 0.212a 0.833 LGE[例(%)] 91(61.1) 24(80.0) 3.114b 0.078 室间隔肥厚[例(%)] 130(87.2) 24(80.0) 0.197b 0.384 心尖部肥厚[例(%)] 14(9.4) 9(30.0) 0.536b 0.005 左心室弥漫性肥厚[例(%)] 38(25.5) 10(33.3) 0.432b 0.511 双心室肥厚[例(%)] 3(2.0) 2(6.7) 0.230b 0.196 心尖部室壁瘤[例(%)] 1(0.7) 4(13.3) 0.512b 0.003 注:a为t值,b为χ2值,c为Z值。 表 2 影响老年nHCM患者OS的多因素Cox回归分析
Table 2. Multivariate Cox regression analysis of factors affecting OS in elderly patients with nHCM
变量 β SE Waldχ2 P值 HR(95% CI) Gal-3 1.114 0.160 48.664 0.001 3.047(2.228~4.116) 室性心动过速 0.995 0.406 6.012 0.014 2.705(1.221~5.991) LGE 1.008 0.504 3.996 0.046 2.740(1.020~7.360) 运动负荷试验 1.013 0.446 5.153 0.023 2.753(1.148~6.601) 心尖部室壁瘤 1.907 0.559 11.662 < 0.001 6.735(2.254~20.127) -
[1] DE MARVAO A, MCGURK K A, ZHENG S L, et al. Phenotypic expression and outcomes in individuals with rare genetic variants of hypertrophic cardiomyopathy[J]. J Am Coll Cardiol, 2021, 78(11): 1097-1110. doi: 10.1016/j.jacc.2021.07.017 [2] MARON B J, DESAI M Y, NISHIMURA R A, et al. Diagnosis and evaluation of hypertrophic cardiomyopathy: JACC state-of-the-art review[J]. J Am Coll Cardiol, 2022, 79(4): 372-389. doi: 10.1016/j.jacc.2021.12.002 [3] LIU J, WU G X, ZHANG C, et al. Improvement in sudden cardiac death risk prediction by the enhanced American College of Cardiology/American Heart Association strategy in Chinese patients with hypertrophic cardiomyopathy[J]. Heart Rhythm, 2020, 17(10): 1658-1663. doi: 10.1016/j.hrthm.2020.04.017 [4] WEISSLER-SNIR A, ALLAN K, CUNNINGHAM K, et al. Hypertrophic cardiomyopathy-related sudden cardiac death in young people in Ontario[J]. Circulation, 2019, 140(21): 1706-1716. doi: 10.1161/CIRCULATIONAHA.119.040271 [5] GOFF Z D, CALKINS H. Sudden death related cardiomyopathies-arrhythmogenic right ventricular cardiomyopathy, arrhythmogenic cardiomyopathy, and exercise-induced cardiomyopathy[J]. Prog Cardiovasc Dis, 2019, 62(3): 217-226. doi: 10.1016/j.pcad.2019.04.002 [6] CHOI Y J, CHOI E K, HAN K D, et al. Temporal trends of the prevalence and incidence of atrial fibrillation and stroke among Asian patients with hypertrophic cardiomyopathy: a nationwide population-based study[J]. Int J Cardiol, 2018, 273: 130-135. doi: 10.1016/j.ijcard.2018.08.038 [7] 陈景钗, 汪荣华, 欧阳元付. 超声心动图检查对肥厚型心肌病的临床意义[J]. 中华全科医学, 2014, 12(5): 794-795. https://www.cnki.com.cn/Article/CJFDTOTAL-SYQY201405054.htmCHEN J C, WANG R H, OUYANG Y F. Clinical significances of echocardiography examination in patients with hypertrophic cardiomyopathy[J]. Chinese Journal of General Practice, 2014, 12(5): 794-795. https://www.cnki.com.cn/Article/CJFDTOTAL-SYQY201405054.htm [8] ELLIOTT P M, ANASTASAKIS A, BORGER M A, et al. 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC)[J]. Eur Heart J, 2014, 35(39): 2733-2779. doi: 10.1093/eurheartj/ehu284 [9] OMMEN S R, MITAL S, BURKE M A, et al. 2020 AHA/ACC Guideline for the Diagnosis and Treatment of Patients with Hypertrophic Cardiomyopathy: Executive Summary: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines[J]. J Am Coll Cardiol, 2020, 76(25): 3022-3055. doi: 10.1016/j.jacc.2020.08.044 [10] 朱峰. 《中国成人肥厚型心肌病诊断与治疗指南2023》要点解读[J]. 临床心血管病杂志, 2023, 39(6): 413-416. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202306002.htmZHU F. An essential introduction to the 2023 guideline for diagnosis and treatment patients with hypertrophic cardiomyopathy[J]. Journal of Clinical Cardiology, 2023, 39(6): 413-416. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202306002.htm [11] SEGEV A, WASSERSTRUM Y, ARAD M, et al. Ventricular arrhythmias in patients with hypertrophic cardiomyopathy: prevalence, distribution, predictors, and outcome[J]. Heart Rhythm, 2023, 20(10): 1385-1392. doi: 10.1016/j.hrthm.2023.06.015 [12] SONG Y Y, BI X Y, CHEN L, et al. Reduced myocardial septal function assessed by cardiac magnetic resonance feature tracking in patients with hypertrophic obstructive cardiomyopathy: associated with histological myocardial fibrosis and ventricular arrhythmias[J]. Eur Heart J Cardiovasc Imaging, 2022, 23(8): 1006-1015. doi: 10.1093/ehjci/jeac032 [13] VARNAVA A M, ELLIOTT P M, MAHON N, et al. Relation between myocyte disarray and outcome in hypertrophic cardiomyopathy[J]. Am J Cardiol, 2001, 88(3): 275-279. doi: 10.1016/S0002-9149(01)01640-X [14] HAMAD A K S. Risk of sudden cardiac death and preventive measures in athletes[J]. Int J Cardiol, 2022, 8(4): 89. [15] KAMP N J, CHERY G, KOSINSKI A S, et al. Risk stratification using late gadolinium enhancement on cardiac magnetic resonance imaging in patients with hypertrophic cardiomyopathy: a systematic review and meta-analysis[J]. Prog Cardiovasc Dis, 2021, 66: 10-16. doi: 10.1016/j.pcad.2020.11.001 [16] WENG Z, YAO J L, CHAN R H, et al. Prognostic value of LGE-CMR in HCM: a meta-analysis[J]. JACC Cardiovasc Imaging, 2016, 9(12): 1392-1402. doi: 10.1016/j.jcmg.2016.02.031 [17] CHAN R H, MARON B J, OLIVOTTO I, et al. Prognostic value of quantitative contrast-enhanced cardiovascular magnetic resonance for the evaluation of sudden death risk in patients with hypertrophic cardiomyopathy[J]. Circulation, 2014, 130(6): 484-495. doi: 10.1161/CIRCULATIONAHA.113.007094 [18] MENTIAS A, RAEISI-GIGLOU P, SMEDIRA N G, et al. Late gadolinium enhancement in patients with hypertrophic cardiomyopathy and preserved systolic function[J]. J Am Coll Cardiol, 2018, 72(8): 857-870. doi: 10.1016/j.jacc.2018.05.060 [19] XU J, ZHUANG B Y, SIRAJUDDIN A, et al. MRI T1 mapping in hypertrophic cardiomyopathy: evaluation in patients without late gadolinium enhancement and hemodynamic obstruction[J]. Radiology, 2020, 294(2): 275-286. doi: 10.1148/radiol.2019190651 [20] IGARASHI M, NOGAMI A, KUROSAKI K, et al. Radiofrequency catheter ablation of ventricular tachycardia in patients with hypertrophic cardiomyopathy and apical aneurysm[J]. JACC Clin Electrophysiol, 2018, 4(3): 339-350. doi: 10.1016/j.jacep.2017.12.020 [21] TRIPPEL T D, MENDE M, DÜNGEN H D, et al. The diagnostic and prognostic value of galectin-3 in patients at risk for heart failure with preserved ejection fraction: results from the DIAST-CHF study[J]. ESC Heart Fail, 2021, 8(2): 829-841. doi: 10.1002/ehf2.13174 [22] EMET S, DADASHOV M, SONSOZ M R, et al. Galectin-3: a novel biomarker predicts sudden cardiac death in hypertrophic cardiomyopathy[J]. Am J Med Sci, 2018, 356(6): 537-543. doi: 10.1016/j.amjms.2018.08.013 [23] AGUIAR ROSA S, ROCHA LOPES L, FIARRESGA A, et al. Coronary microvascular dysfunction in hypertrophic cardiomyopathy: pathophysiology, assessment, and clinical impact[J]. Microcirculation, 2021, 28(1): e12656. DOI: 10.1111/micc.12656. [24] CECCHI F, OLIVOTTO I, GISTRI R, et al. Coronary microvascular dysfunction and prognosis in hypertrophic cardiomyopathy[J]. N Engl J Med, 2003, 349(11): 1027-1035. doi: 10.1056/NEJMoa025050 -





 下载:
下载: