Development of a prediction model for enteral feeding intolerance in patients with sepsis
-
摘要:
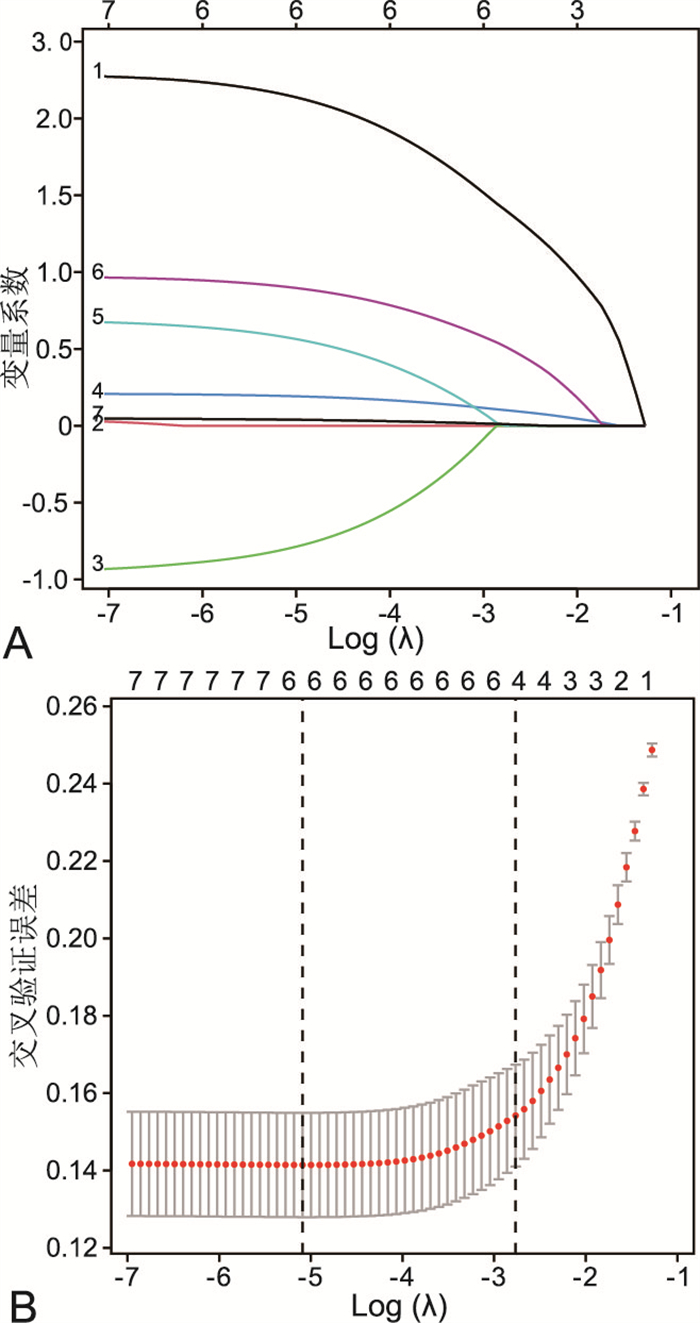
目的 探讨脓毒症患者肠内喂养不耐受(EFI)的危险因素,了解脓毒症患者EFI的发生情况。构建脓毒症患者发生EFI的风险预测模型,便于高危人群的筛查,以防控EFI的发生。 方法 采用方便抽样法选取2022年1月—2023年6月新疆某三级甲等医院重症医学科收治的行肠内营养治疗的脓毒症患者作为研究对象,以患者是否发生EFI分为喂养耐受组和喂养不耐受组,对患者的一般资料、临床资料、喂养不耐受相关资料进行单因素分析,应用LASSO回归解决各变量间的共线性问题,将LASSO回归分析结果中的变量纳入logistic回归分析,得出脓毒症患者发生EFI的危险因素,并基于此构建脓毒症患者EFI风险预测模型,绘制列线图、ROC曲线、决策曲线、校准曲线,对预测模型的诊断效能进行评价及验证。 结果 共纳入199例行肠内营养治疗的脓毒症患者,其中不耐受组93例,耐受组106例,EFI发生率为46.7%。多因素分析显示序贯性器官功能衰竭(SOFA)评分、营养风险筛查2002(NRS-2002)评分、镇痛剂、ICU住院时间是脓毒症患者发生EFI的独立影响因素。ROC曲线分析显示,脓毒症患者发生EFI的曲线下面积为0.885(95% CI:0.833~0.933),最大约登指数为0.689,敏感度为0.849,特异度为0.839。 结论 SOFA评分、NRS-2002评分、镇痛剂、ICU住院时间是脓毒症患者发生EFI的影响因素,基于此构建的风险预测模型,经验证后发现该模型可较准确地预测脓毒症患者发生EFI的风险,有助于临床医护人员对患者进行科学、个体化的肠内营养治疗。 Abstract:Objective To explore the risk factors of enteral feeding intolerance (EFI) in sepsis patients and to understand the occurrence of EFI in sepsis patients. To construct a risk prediction model for the occurrence of EFI in sepsis patients to facilitate the screening of high-risk groups to prevent and control the occurrence of EFI. Methods Convenience sampling method was used to select sepsis patients admitted to the Department of Critical Care Medicine of a tertiary-level hospital in Xinjiang who underwent enteral nutrition therapy from January 2022 to June 2023 as study subjects and were divided into the feeding tolerance group and feeding intolerance group by whether or not EFI occurred in the patients, and a one-way analysis was carried out on the patients ' general, clinical, and feeding intolerance-related data, and LASSO regression was applied to solve the covariance problem among variables, then the variables in the results of LASSO regression analysis were included in logistic regression analysis to derive the risk factors for EFI in patients with sepsis, on the basis of which we constructed a prediction model for the risk of EFI in patients with sepsis, and plotted a Nomogram, ROC curve, decision curve analysis, and calibration curve to evaluate and validate the diagnostic efficacy of the prediction model. Results A total of 199 sepsis patients with enteral nutrition therapy were included, including 93 cases in the intolerant group and 106 cases in the tolerant group, and the incidence rate of EFI was 46.7%. Multifactorial analysis showed that sequential organ failure assessment (SOFA) score, nutritional risk screening (NRS-2002) score, analgesics, and ICU length of stay were independent risk factors for the occurrence of EFI in patients with sepsis. The area under the ROC curve was 0.885 (95% CI: 0.833-0.933), and the maximal Youden index was 0.689, with a sensitivity of 0.849, and a specificity of 0.839. Conclusion SOFA score, NRS-2002 score, analgesics, and ICU length of stay are risk factors for EFI in septic patients. The risk prediction model constructed in this study based on this was validated and found to be a more accurate predictor of the risk of EFI in patients with sepsis, which can help clinical healthcare professionals provide scientific and individualized enteral nutrition therapy to patients. -
Key words:
- Sepsis /
- Enteral feeding intolerance /
- Prediction model
-
表 1 2组脓毒症患者一般资料比较
Table 1. Comparison of clinical data between two groups of sepsis patients
项目 耐受组(n=106) 不耐受组(n=93) 统计量 P值 项目 耐受组(n=106) 不耐受组(n=93) 统计量 P值 性别[例(%)] 0.895a 0.344 镇痛剂[例(%)] 43.983a < 0.001 男性 75(70.8) 59(63.4) 否 75(70.8) 22(23.7) 女性 31(29.2) 34(36.6) 是 31(29.2) 71(76.3) 年龄(x±s, 岁) 59.0±17.2 76.2±10.1 8.693b < 0.001 使用抗菌药物种类[例(%)] 0.103a 0.748 基础疾病[例(%)] 0.178a 0.672 < 2 22(20.8) 22(23.7) 无 17(16.0) 12(12.9) ≥2 84(79.2) 71(76.3) 有 89(84.0) 81(87.1) 抑酸剂[例(%)] 0.211a 0.646 NRS-2002评分[例(%)] 59.938a < 0.001 否 40(37.7) 39(41.9) < 3 75(70.8) 14(15.1) 是 66(62.3) 54(58.1) ≥3 31(29.2) 79(84.9) 营养液类型[例(%)] 1.507a 0.471 mNUTRIC评分[例(%)] 8.200a 0.007 短肽类 69(65.1) 68(73.1) < 5 33(31.1) 13(14.0) 整蛋白类 33(31.1) 22(23.7) ≥5 73(68.9) 80(86.0) 短肽+整蛋白 4(3.8) 3(3.2) APACHEⅡ评分[例(%)] 0.026a 0.873 血清白蛋白[例(%)] 2.192a 0.146 < 20 57(53.8) 52(55.9) ≥35 g/L 45(42.5) 30(32.3) ≥20 49(46.2) 41(44.1) < 35 g/L 61(57.5) 63(67.7) SOFA评分[M(P25, P75), 分] 7(5, 12) 12(10, 15) -6.799c < 0.001 血红蛋白(x±s, g/L) 103.6±32.9 108.1±27.9 1.036b 0.307 CRRT[例(%)] 4.271a 0.040 白细胞计数[M(P25, P75),×109/L] 13.3(10.5, 16.9) 13.1(9.4, 16.9) -0.419c 0.675 否 70(66.0) 48(51.6) ICU住院时间[M(P25, P75),d] 12(7, 17) 14(9, 22) -2.777c 0.005 是 36(34.0) 45(48.4) 机械通气时间[M(P25, P75),d] 11(7, 15) 11(8, 17) -0.983c 0.325 注:a为χ2值,b为t值, c为Z值。 表 2 变量赋值情况
Table 2. Variable assignment
变量 赋值方法 年龄 以实际值赋值 SOFA评分 以实际值赋值 ICU住院时间 以实际值赋值 NRS-2002评分 <3分=0,≥3分=1 mNUTRIC评分 <5分=0,≥5分=1 CRRT 否=0,是=1 镇痛剂 否=0,是=1 表 3 脓毒症患者肠内喂养不耐受危险因素的logistic多因素回归分析
Table 3. Logistic multivariable regression analysis of risk factors for enteral feeding intolerance
预测变量 B SE Waldχ2 P值 OR值 95% CI NRS-2002评分 2.104 0.437 23.142 < 0.001 8.199 3.479~19.322 SOFA评分 0.191 0.048 15.880 < 0.001 1.210 1.102~1.329 镇痛剂 0.948 0.414 5.236 0.022 2.580 1.146~5.810 ICU住院时间 0.044 0.019 5.510 0.019 1.045 1.007~1.085 -
[1] SINGER M, DEUTSCHMAN C S, SEYMOUR C W, et al. The third international consensus definitions for sepsis and septic shock(Sepsis-3)[J]. JAMA, 2016, 315(8): 801-810. doi: 10.1001/jama.2016.0287 [2] MUKHOPADHYAY A, TAN Z Y, CHEONG S H L, et al. Differential effects of early energy and protein inadequacies on the outcome of critically ill patients[J]. Nutr Clin Pract, 2021, 36(2): 456-463. doi: 10.1002/ncp.10543 [3] ABUGROUN A, NAYYAR A, ABDEL-RAHMAN M, et al. Impact of malnutrition on hospitalization outcomes for older adults admitted for sepsis[J]. Am J Med, 2021, 134(2): 221-226. e1. doi: 10.1016/j.amjmed.2020.06.044 [4] MCLAUGHLIN J, CHOWDHURY N, DJURKOVIC S, et al. Clinical outcomes and financial impacts of malnutrition in sepsis[J]. Nutr Health, 2020, 26(3): 175-178. doi: 10.1177/0260106020930145 [5] 华美芳, 陈莉. 鼻肠管用于神经外科重症机械通气患者的效果研究[J]. 现代医药卫生, 2019, 35(22): 3512-3514. doi: 10.3969/j.issn.1009-5519.2019.22.033HUA M F, CHEN L. Study of the effect of nasointestinal tubes in neurosurgical intensive mechanical ventilation patients[J]. J Mod Med Health, 2019, 35(22): 3512-3514. doi: 10.3969/j.issn.1009-5519.2019.22.033 [6] 亚洲急危重症协会中国腹腔重症协作组. 重症病人胃肠功能障碍肠内营养专家共识(2021版)[J]. 中华消化外科杂志, 2021, 20(11): 1123-1136. doi: 10.3760/cma.j.cn115610-20211012-00497Chinese Abdominal Intensive Care Association, Asia Society for Emergency and Critical Care Medicine. Expert consensus on enteral nutrition for gastrointestinal dysfunction in critically ill patients (2021 edition)[J]. Chin J Dig Surg, 2021, 20(11): 1123-1136. doi: 10.3760/cma.j.cn115610-20211012-00497 [7] 张丽华, 张莉, 张丽萍, 等. 脓毒症患者肠内营养喂养不耐受现况及影响因素研究[J]. 华南预防医学, 2023, 49(2): 174-178. https://www.cnki.com.cn/Article/CJFDTOTAL-GDWF202302011.htmZHANG L H, ZHANG L, ZHANG L P, et al. Enteral nutrition feeding intolerance and its influencing factors in patients with sepsis[J]. South China J Prev Med, 2023, 49(2): 174-178. https://www.cnki.com.cn/Article/CJFDTOTAL-GDWF202302011.htm [8] 向艳, 金静芬, 王丽竹, 等. 脓毒症患者肠内营养不耐受现状及影响因素分析[J]. 护理与康复, 2022, 21(7): 12-16, 22. doi: 10.3969/j.issn.1671-9875.2022.07.003XIANG Y, JIN J F, WANG L Z, et al. Present status on enteral nutrition intolerance for septic patients and analysis on influencing factor[J]. Nursing and Rehabilitation Journal, 2022, 21(7): 12-16, 22. doi: 10.3969/j.issn.1671-9875.2022.07.003 [9] HU K L, DENG X L, HAN L, et al. Development and validation of a predictive model for feeding intolerance in intensive care unit patients with sepsis[J]. Saudi J Gastroenterol, 2021, 28(1): 32-38. [10] 周田田. 老年脓毒症患者肠内营养喂养不耐受的相关因素分析及护理对策[D]. 镇江: 江苏大学, 2018.ZHOU T T. The nursing countermeasures and analysis of related factors with enteral feeding intolerance in elderly septic patients[D]. Zhenjiang: Jiangsu University, 2018. [11] 郭林彬, 高薇薇, 高万朋, 等. 脓毒症急性胃肠损伤治疗研究进展[J]. 中国临床研究, 2023, 36(10): 1504-1508. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGCK202310013.htmGUO L B, GAO W W, GAO W P, et al. Progress in the treatment of acute gastrointestinal injury in sepsis[J]. Chinese Journal of Clinical Research, 2023, 36(10): 1504-1508. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGCK202310013.htm [12] JENKINS B, CALDER P C, MARINO L V. A systematic review of the definitions and prevalence of feeding intolerance in critically ill adults[J]. Clin Nutr ESPEN, 2022, 49: 92-102. doi: 10.1016/j.clnesp.2022.04.014 [13] YU K R, GUO N, ZHANG D D, et al. Prevalence and risk factors of enteral nutrition intolerance in intensive care unit patients: a retrospective study[J]. Chin Med J(Engl), 2022, 135(15): 1814-1820. [14] 伏添, 王彩凤, 张谞丰, 等. SAP患者早期肠内营养过程FI的预测评估[J]. 昆明医科大学学报, 2019, 40(12): 108-113. doi: 10.3969/j.issn.1003-4706.2019.12.022FU T, WANG C F, ZHANG X F, et al. The predictive assessment of feeding intolerance during early enteral nutrition in patients with severe acute pancreatitis[J]. Journal of Kunming Medical University, 2019, 40(12): 108-113. doi: 10.3969/j.issn.1003-4706.2019.12.022 [15] 刘炳炜, 徐燕平, 席绍松, 等. SOFA评分联合PCT检测对脓毒症患者病情及其预后的临床评估价值[J]. 中华全科医学, 2021, 19(3): 391-393. doi: 10.16766/j.cnki.issn.1674-4152.001818LIU B W, XU Y P, XI S S, et al. Clinical value of SOFA combined with procalcitonin test in assessing the condition and prognosis of patients with sepsis[J]. Chinese Journal of General Practice, 2021, 19(3): 391-393. doi: 10.16766/j.cnki.issn.1674-4152.001818 [16] LI J B, WANG L J, ZHANG H, et al. Different definitions of feeding intolerance and their associations with outcomes of critically ill adults receiving enteral nutrition: a systematic review and meta-analysis[J]. J Intensive Care, 2023, 11(1): 29. doi: 10.1186/s40560-023-00674-3 [17] 苏小平, 徐静娟, 赵亚东, 等. 危重患者早期肠内营养喂养不耐受风险预测模型的构建[J]. 护理学报, 2022, 29(17): 47-51. https://www.cnki.com.cn/Article/CJFDTOTAL-NFHL202217009.htmSU X P, XU J J, ZHAO Y D, et al. Construction of a prediction model for the risk of intolerance to early enteral nutrition feeding in critically ill patients[J]. Journal of Nursing, 2022, 29(17): 47-51. https://www.cnki.com.cn/Article/CJFDTOTAL-NFHL202217009.htm [18] XIAO Y J, XU L. Prevalence and risk factors of enteral feeding intolerance in critically ill patients and the effectiveness of preventive treatments: a prospective study[J]. Saudi J Med Med Sci, 2023, 11(2): 135-142. doi: 10.4103/sjmms.sjmms_384_22 [19] DICKERSON R N, FARRAR J E, BYERLY S, et al. Enteral feeding tolerance during pharmacologic neuromuscular blockade[J]. Nutr Clin Pract, 2023, 38(6): 1236-1246. doi: 10.1002/ncp.11045 [20] 范小宁, 孙盼盼, 靳玉萍, 等. 护士主导的肠内营养喂养策略在神经重症患者中的应用[J]. 中华全科医学, 2022, 20(12): 2151-2155. doi: 10.16766/j.cnki.issn.1674-4152.002791FAN X N, SUN P P, JIN Y P, et al. Application of nurse-led enteral nutritional feeding strategies in neurological intensive care unit patients[J]. Chinese Journal of General Practice, 2022, 20(12): 2151-2155. doi: 10.16766/j.cnki.issn.1674-4152.002791 [21] HEYLAND D K, ORTIZ A, STOPPE C, et al. Incidence, risk factors, and clinical consequence of enteral feeding intolerance in the mechanically ventilated critically ill: an analysis of a multicenter, multiyear database[J]. Crit Care Med, 2021, 49(1): 49-59. -





 下载:
下载: