Analysis of the difference of intestinal flora between patients with perianal abscess before and after surgery and healthy people
-
摘要:
目的 通过16S rDNA基因测序检测肛周脓肿患者手术前后的肠道菌群分布,探讨其与健康人的菌群分布是否存在差异。 方法 收集2022年8—11月期间在浙江中医药大学附属嘉兴中医院肛肠科就诊的15名肛周脓肿患者(观察组)及15名健康体检者(对照组)的临床资料,提取其粪便DNA,通过PCR扩增和16S rDNA基因测序,进行Alpha多样性、Beta多样性等数据分析,并筛选肛周脓肿可能的主要标志菌群。 结果 Alpha多样性分析表明,与对照组相比,观察组术前的Chao1和Observed_species指数升高,术后的Shannon和Simpson指数降低,差异均有统计学意义(P < 0.05);与术前比较,观察组术后的Chao1、Shannon、Simpson、Observed_species指数均降低(P < 0.05)。厚壁菌门、变形菌门、放线菌门和拟杆菌门的相对丰度在对照组、观察组术前、术后之间差异有统计学意义(P < 0.05),与对照组相比,观察组术前放线菌门的相对丰度降低(P < 0.05),术后变形菌门的相对丰度增加(P < 0.05);与术前比较,观察组术后变形菌门的相对丰度增加(P < 0.05)。筛选肛周脓肿主要标志菌群,ROC曲线分析显示,嗜胆菌属的AUC最大(AUC=0.831)。 结论 肛周脓肿患者手术前后与健康人肠道菌群存在显著差异,手术治疗后肠道菌群丰度发生显著变化,嗜胆菌属可能是肛周脓肿的主要标志菌群。 -
关键词:
- 肛周脓肿 /
- 肠道菌群 /
- 16S rDNA测序
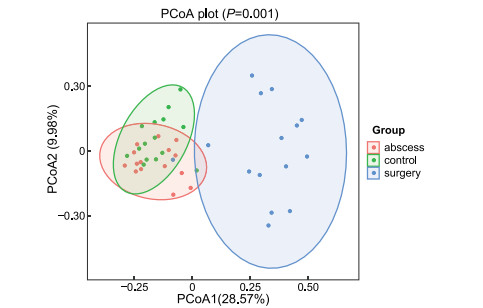
Abstract:Objective The intestinal flora distribution of perianal abscess patients before and after surgery was detected by 16S rDNA gene sequencing to explore whether the flora distribution was different from that of healthy people. Methods Clinical data of 15 patients with perianal abscess (observation group) and 15 healthy individuals (control group) who visited the Department of Anorectal of Jiaxing Hospital of Traditional Chinese Medicine Affiliated to Zhejiang Chinese Medicine University between August and November 2022 were collected, their fecal DNA was extracted, and their data including alpha diversity, beta diversity were analyzed by PCR amplification and 16S rDNA gene sequencing, and possible major hallmark flora of perianal abscess were screened. Results Alpha diversity analysis showed that compared to the control group, the observation group had preoperative levels of Chao1 and Observed_species increased, while the postoperative Shannon and Simpson indices decreased, with significant differences (P < 0.05). Compared with operative, postoperative Chao1, Shannon, Simpson, Observed_species in the observation decreased (P < 0.05). The relative abundance of Bacillota, Pseudomonadota, Actinomycetota and Bacteroidota was significantly different between the control group and the observation group before and after surgery (P < 0.05). Compared with the control group, the relative abundance of Actinomycetota in the observation group before surgery was reduced (P < 0.05), and the relative abundance of Pseudomonadota after surgery was increased (P < 0.05). Compared with operative, the relative abundance of Pseudomonadota in the observation increased after operation (P < 0.05). The main marker flora of perianal abscess was screened, and receiver operating characteristic analysis showed that Bilophila wadsworthia had the max AUC (AUC=0.831). Conclusion The intestinal flora of patients with perianal abscess differs significantly from that of healthy individuals before and after surgery, and the abundance of intestinal flora changes significantly after surgical treatment. Bilophila may be a major marker of perianal abscess. -
Key words:
- Perianal abscess /
- Intestinal flora /
- 16S rDNA gene sequencing
-
表 1 2组受试者肠道微生物群多样性的Alpha指数比较[M(P25, P75)]
Table 1. Alpha index comparison of intestinal microbiota diversity between two groups[M(P25, P75)]
组别 时间 例数 Chao1指数 Shannon指数 Simpson指数 Observed_species指数 观察组 术前 15 80.00(59.13, 104.63) 4.57(4.36, 4.80) 0.92(0.90, 0.93) 80.00(59.00, 98.50) 术后 15 34.00(24.00, 60.58) 2.40(2.05, 3.09) 0.66(0.55, 0.81) 34.00(24.00, 59.50) 对照组 15 54.00(42.80, 72.13) 4.51(3.47, 4.79) 0.93(0.87, 0.94) 54.00(42.50, 72.00) Z值a 2.556 3.011 2.414 2.544 P值a 0.011 0.003 0.016 0.011 Z值b 2.448 0.768 0.042 2.386 P值b 0.013 0.461 0.967 0.016 Z值c 1.722 3.609 3.553 1.931 P值c 0.089 < 0.001 < 0.001 0.056 注:a为观察组术前与术后比较;b为观察组术前与对照组比较;c为观察组术后与对照组比较。 表 2 2组受试者肠道门水平细菌相对丰度比较[M(P25, P75)]
Table 2. Comparison of relative abundance of bacteria at intestinal portal level between the two groups[M(P25, P75)]
组别 时间 例数 厚壁菌门 变形菌门 放线菌门 拟杆菌门 观察组 术前 15 59.55(45.51, 76.81) 12.38(4.22, 27.84) 2.62(1.20, 4.60) 8.43(3.40, 14.41) 术后 15 16.34(9.63, 29.89) 73.17(45.83, 82.58) 1.31(0.23, 6.35) 0.00(0.00, 2.78) 对照组 15 56.72(27.75, 69.05) 13.17(6.81, 22.88) 13.79(6.50, 21.32) 5.25(2.31, 16.13) Z值a 2.779 2.783 0.454 2.013 P值a 0.005 0.005 0.651 0.035 Z值b 1.016 0.021 2.924 0.643 P值b 0.325 0.001 0.003 0.539 Z值c 3.049 4.086 3.090 2.544 P值c 0.002 < 0.001 0.001 0.011 注:a为观察组术前与术后比较;b为观察组术前与对照组比较;c为观察组术后与对照组比较。 表 3 2组受试者肠道属水平细菌相对丰度比较[M(P25, P75)]
Table 3. Comparison of the relative abundance of intestinal bacteria at the genus level between the two groups[M(P25, P75)]
组别 时间 例数 大肠杆菌属 伯克霍尔德菌属 双歧杆菌属 粪杆菌属 巨单胞菌属 观察组 术前 15 1.48(0.49, 9.00) 1.58(0.84, 4.67) 1.00(0.20, 18.03) 11.91(0.20, 18.03) 0.00(0.00, 4.72) 术后 15 20.21(0.06, 39.35) 9.27(3.83, 21.79) 0.06(0.00, 5.90) 0.00(0.00, 0.08) 0.00(0.00, 0.00) 对照组 15 1.44(0.25, 8.23) 1.74(1.15, 5.46) 8.26(3.53, 20.52) 4.82(0.29, 13.38) 0.00(0.00, 9.33) Z值a 0.852 2.669 0.031 3.061 1.048 P值a 0.391 0.010 0.982 < 0.001 0.301 Z值b 0.333 0.477 2.843 0.457 0.619 P值b 0.744 0.653 0.004 0.653 0.595 Z值c 1.141 2.675 1.934 3.469 2.225 P值c 0.267 0.007 0.081 < 0.001 0.074 组别 时间 例数 拟杆菌属 链球菌属 肠球菌属 瘤胃球菌属 观察组 术前 15 3.31(1.80, 8.58) 0.45(0.12, 1.47) 0.00(0.00, 0.00) 0.79(0.12, 2.61) 术后 15 0.00(0.00, 1.40) 1.69(0.34, 6.43) 5.32(0.60, 15.52) 0.00(0.00, 0.00) 对照组 15 2.77(0.97, 8.66) 0.36(0.03, 1.10) 0.00(0.00, 0.00) 0.75(0.11, 1.67) Z值a 2.001 1.538 3.296 3.140 P值a 0.048 0.124 < 0.001 < 0.001 Z值b 0.394 0.376 1.002 0.415 P值b 0.713 0.713 0.775 0.683 Z值c 2.553 1.812 4.727 3.525 P值c 0.013 0.074 < 0.001 0.001 注:a为观察组术前与术后比较;b为观察组术前与对照组比较;c为观察组术后与对照组比较。 -
[1] WANG J P, CAI C, DU J L, et al. Role of interleukin-17 in the pathogenesis of perianal abscess and anal fistula: a clinical study on 50 patients with perianal abscess[J]. ANZ J Surg, 2019, 89(3): 244-247. doi: 10.1111/ans.14874 [2] 中国医师协会肛肠医师分会指南工作委员会. 肛周脓肿临床诊治中国专家共识[J]. 中华胃肠外科杂志, 2018, 21(4): 456-457.Guide Working Committee of the Anal and Intestinal Doctors Branch of the Chinese Medical Association. Chinese expert consensus on clinical diagnosis and treatment of perianal abscess[J]. Chinese Journal of Gastroenterology, 2018, 21(4): 456-457. [3] GAERTNER W B, BURGESS P L, DAVIDS J S, et al. The American society of colon and rectal surgeons clinical practice guidelines for the management of anorectal abscess, Fistula-in-Ano, and rectovaginal fistula[J]. Dis Colon Rectum, 2022, 65(8): 964-985. doi: 10.1097/DCR.0000000000002473 [4] PHAM V T, DOLD S, REHMAN A, et al. Vitamins, the gut microbiome and gastrointestinal health in humans[J]. Nutr Res, 2021, 95, 35-53. doi: 10.1016/j.nutres.2021.09.001 [5] 刘莉. 基于菌-肠-脑轴的肠肽与焦虑抑郁关系的研究进展[J]. 中华全科医学, 2022, 20(8): 1388-1391, 1399. doi: 10.16766/j.cnki.issn.1674-4152.002604LIU L. Research progress on the relationship between gut peptide and anxiety and depression based on bacteria-gut brain axis[J]. Chinese Journal of General Practice, 2022, 20(8): 1388-1391, 1399. doi: 10.16766/j.cnki.issn.1674-4152.002604 [6] MA M, LU H M, YANG Z Z, et al. Differences in microbiota between acute and chronic perianal eczema[J]. Medicine(Baltimore), 2021, 100(16): e25623. DOI: 10.1097/MD.0000000000025623. [7] YUAN B, MA B, YU J, et al. Fecal bacteria as non-invasive biomarkers for colorectal adenocarcinoma[J]. Front Oncol, 2021, 11: 664321. DOI: 10.3389/fonc.2021.664321. [8] 王同利, 吴庆, 严红琴, 等. 肛周脓肿病原菌分布及耐药性分析[J]. 中国卫生检验杂志, 2021, 31(12): 1444-1446, 1459. https://www.cnki.com.cn/Article/CJFDTOTAL-ZWJZ202112011.htmWANG T L, WU Q, YAN H Q, et al. Distribution and drug resistance analysis of pathogenic bacteria in perianal abscess[J]. Chinese Journal of Health Inspection, 2021, 31(12): 1444-1446, 1459. https://www.cnki.com.cn/Article/CJFDTOTAL-ZWJZ202112011.htm [9] 陈孝平, 汪建平, 赵继宗. 外科学[M]. 9版. 北京: 人民卫生出版社, 2018: 399-400.CHEN X P, WANG J P, ZHAO J Z. Surgery[M]. 9th edition. Beijing: People' s Health Publishing House, 2018: 399-400. [10] 马晔琳, 钱晓玲, 杨敏春. 中老年痰湿质人群肠道菌群结构特征研究[J]. 中华全科医学, 2020, 18(1): 113-118. doi: 10.16766/j.cnki.issn.1674-4152.001182MA Y L, QIAN X L, YANG M C. Study on the structural characteristics of intestinal microflora in middle-aged and elderly people with phlegm and dampness[J]. Chinese Journal of General Practice, 2020, 18(1): 113-118. doi: 10.16766/j.cnki.issn.1674-4152.001182 [11] BÁLINT A, FARKAS K, MÉHI O, et al. Functional anatomical changes in ulcerative colitis patients determine their gut microbiota composition and consequently the possible treatment outcome[J]. Pharmaceuticals(Basel), 2020, 13(11): 346. doi: 10.3390/ph13110346 [12] 唐琳, 刘波. 肠道菌群在结直肠癌发病与治疗中的研究进展[J]. 山东医药, 2022, 62(10): 101-104. https://www.cnki.com.cn/Article/CJFDTOTAL-SDYY202210025.htmTANG L, LIU B. Research progress of intestinal flora in the pathogenesis and treatment of colorectal cancer[J]. Shandong Medical Journal, 2022, 62(10): 101-104. https://www.cnki.com.cn/Article/CJFDTOTAL-SDYY202210025.htm [13] YUE B, LUO X P, YU Z L, et al. Inflammatory bowel disease: a potential result from the collusion between gut microbiota and mucosal immune system[J]. Microorganisms, 2019, 7(10): 440. doi: 10.3390/microorganisms7100440 [14] 蒋宇. 肛周脓肿患者病情严重程度与纤维蛋白原、D-二聚体水平相关性分析[J]. 中国临床医学, 2020, 27(5): 841-843. https://www.cnki.com.cn/Article/CJFDTOTAL-LCYX202005026.htmJIANG Y. Correlation analysis between severity of patients with perianal abscess and fibrinogen and D-dimer levels[J]. Chinese Journal of Clinical Medicine, 2020, 27(5): 841-843. https://www.cnki.com.cn/Article/CJFDTOTAL-LCYX202005026.htm [15] 郭仕辉, 余永涛, 万佳宏, 等. 变形菌门与哺乳动物结肠肠道菌群失调相关研究进展[J]. 中国微生态学杂志, 2022, 34(4): 479-484. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGWS202204021.htmGUO S H, YU Y T, WAN J H, et al. Research progress in the relationship between Proteus and intestinal flora imbalance in mammals[J]. Chinese Journal of Microbiology, 2022, 34(4): 479-484. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGWS202204021.htm [16] MAHARSHAK N, RINGEL Y, KATIBIAN D, et al. Fecal and mucosa-associated intestinal microbiota in patients with diarrhea-predominant irritable bowel syndrome[J]. Dig Dis Sci, 2018, 63(7): 1890-1899. doi: 10.1007/s10620-018-5086-4 [17] 徐宝琪, 张燕红, 李伊倩. 溃疡性结肠炎患者不同发病状态肠道菌群、炎症因子变化及优势菌敏感性抗菌药物分析[J]. 中华实验和临床感染病杂志, 2020, 14(1): 51-56. https://www.cnki.com.cn/Article/CJFDTOTAL-ZSGR202001009.htmXU B Q, ZHANG Y H, LI Y Q. Analysis of intestinal flora, inflammatory factor changes and antimicrobial susceptibility of dominant bacteria in patients with ulcerative colitis at different stages[J]. Chinese Journal of Experimental and Clinical Infectious Diseases, 2020, 14(1): 51-56. https://www.cnki.com.cn/Article/CJFDTOTAL-ZSGR202001009.htm [18] WALKER A, SCHMITT-KOPPLIN P. The role of fecal sulfur metabolome in inflammatory bowel diseases. International journal of medical microbiology[J]. Int J Med Microbiol, 2021, 311(5): 151513. DOI: 10.1016/j.ijmm.2021.151513. [19] DAHMUS J D, KOTLER D L, KASTENBERG D M, et al. The gut microbiome and colorectal cancer: a review of bacterial pathogenesis[J]. J Gastrointest Oncol, 2018, 9(4): 769-777. doi: 10.21037/jgo.2018.04.07 [20] RIBALDONE D G, PELLICANO R, ACTIS G C. Inflammation: a highly conserved, Janus- like phenomenon-a gastroenterologist' perspective[J]. J Mol Med(Berl), 2018, 96(9): 861-871. -





 下载:
下载: