Influencing factors of dysphagia in the elderly in nursing home: a meta-analysis
-
摘要:
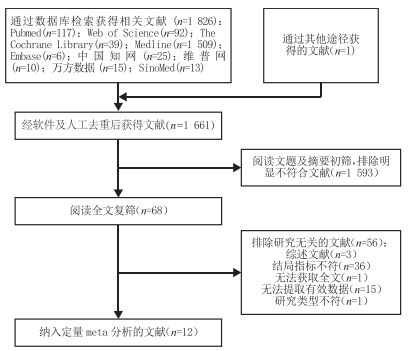
目的 系统评价养老机构老年人发生吞咽障碍的影响因素,为实施针对性干预提供参考。 方法 计算机检索PubMed、Web of Science、The Cochrane Library、Ovid、Embase、CNKI、CBM、WanFang Data以及维普网(VIP)数据库关于养老机构老年人吞咽障碍影响因素的研究,检索时限为建库至2023年3月。2名研究者按照纳入排除标准独立完成文献筛选、数据提取及质量评价,结局指标为养老机构老年人发生吞咽障碍的影响因素(包括其OR值及95% CI)。使用RevMan 5.3软件进行meta分析。 结果 共纳入12篇文献,包括32 890例研究对象。Meta分析结果显示:高龄(P=0.010)、进食时间长(P < 0.001)、进食量少(P=0.007)、协助进食(P < 0.001)、中重度认知障碍(P < 0.001)、脑血管疾病(P=0.040)、心血管疾病(P < 0.001)、肺炎病史(P < 0.001)、牙齿缺失(P < 0.001)、咀嚼困难(P=0.020)和重度依赖(P < 0.001)共11个因素为养老机构老年人吞咽障碍的危险因素。 结论 养老机构老年人发生吞咽障碍的危险因素较多,养老机构工作人员应全面评估老年人的吞咽障碍风险。 Abstract:Objective To systematically evaluate the influencing factors of dysphagia in the elderly in nursing home and provide reference for targeted interventions. Methods Studies on influencing factors of dysphagia among the elderly in nursing home were searched from PubMed, Web of Science, the Cochrane Library, Ovid, Embase, CBM, CNKI, VIP and WanFang Database. The retrieval time was from inception to March 2023. Two researchers screened literature by following the inclusion and exclusion criteria independently, extracted data and evaluated the quality of literature. The influencing factors (including OR value and 95% CI) of dysphagia in the elderly in nursing home were outcome indicators. RevMan 5.3 software was used to conduct meta-analysis. Results The results included a total of 12 studies, including 32890 study subjects. The meta-analysis results showed that advanced age (P=0.010), eating time (long, P < 0.001), food take (less, P=0.007), assisted eating (P < 0.001), moderate to severe cognitive dysfunction (P < 0.001), cerebrovascular disease (P=0.040), cardiovascular disease (P < 0.001), history of pneumonia (P < 0.001), tooth loss (P < 0.001), chewing difficulties (P=0.020), and severe dependence (P < 0.001) were all risk factors for dysphagia in the elderly in nursing homes. Conclusion There are many risk factors for dysphagia among the elderly in nursing homes, and the staff of nursing homes should comprehensively assess the risk of dysphagia among the elderly. -
Key words:
- The aged /
- Nursing home /
- Dysphagia /
- Influencing factors /
- Meta-analysis
-
表 1 纳入研究的基本特征及质量评价
Table 1. Basic information and quality assessment about the included study
作者 年份 地区 样本量 诊断标准 影响因素 质量评价(分) PARK Y H[7] 2013 韩国 395 吞咽功能评估量表 ①②③④⑦⑪⑫⑭ 8 MONCAYO-HERNANDEZ B A[8] 2021 美国 100 容积-粘度测试 ③ 10 XAVIER J S[9] 2022 巴西 73 容积-粘度测试 ①⑤ 10 OKABE Y[10] 2017 日本 238 改良饮水试验 ⑧ 10 HAGGLUND P[11] 2022 瑞典 4 751 询问照护人员 ⑤ 9 CHEN S[12] 2020 中国 775 进食评估问卷 ③⑨⑩ 8 PU D[13] 2017 香港 865 容积-粘度测试+进食评估问卷 ②⑥⑩⑪⑬ 10 刘金枚[14] 2023 中国 475 标准吞咽功能评估量表 ⑧⑪ 10 高薇薇[15] 2019 中国 997 饮水试验 ①②⑧⑨ 10 陈丽丽[16] 2014 中国 400 临床护理用吞咽功能评估工具 ①④⑥⑦⑧⑬ 10 STREICHER M[17] 2017 欧洲和北美 23 549 查阅医疗档案 ⑦⑪⑭⑭ 10 NOGUEIRA D[18] 2023 葡萄牙 272 3盎司水吞咽试验+吞咽困难自评问卷 ① 8 注:①高龄;②性别;③巴塞尔指数;④进食时间(长);⑤进食量(少);⑥协助进食;⑦中重度认知障碍;⑧脑血管疾病;⑨心血管疾病;⑩肺炎病史;⑪重度依赖;⑫ BMI低;⑬牙齿缺失;⑭咀嚼困难。 表 2 养老机构老年人吞咽障碍影响因素的meta分析
Table 2. Meta-analysis of influencing factors of dysphagia in the elderly in nursing home
影响因素 纳入研究 纳入样本量 异质性检验 效应模型 效应量 I2(%) P值 OR(95% CI) P值 高龄 5[7, 9, 15-16, 18] 2 137 92 < 0.001 随机 1.27(1.06~1.53) 0.010 性别(男性) 3[7, 13, 15] 2 257 88 < 0.001 随机 1.11(0.54~2.31) 0.770 进食时间(长) 2[7, 16] 795 0 0.390 固定 3.31(1.94~5.65) < 0.001 进食量(少) 2[9, 11] 4 824 23 0.260 固定 1.88(1.52~2.31) < 0.001 协助进食 2[13, 16] 1 265 0 0.900 固定 3.15(2.19~4.54) < 0.001 中重度认知障碍 3[7, 16-17] 24 344 0 0.400 固定 1.98(1.67~2.36) < 0.001 脑血管疾病 4[10, 14-16] 2 110 97 < 0.001 随机 8.16(1.10~60.26) 0.040 心血管疾病 2[12, 15] 1 772 0 0.840 固定 4.08(2.41~6.89) < 0.001 肺炎病史 2[12, 13] 1 640 0 0.630 固定 4.08(2.18~7.66) < 0.001 BMI(低) 2[7, 17] 23 944 90 0.002 随机 1.74(0.80~3.75) 0.160 咀嚼困难 2[7, 17] 23 944 96 < 0.001 随机 5.33(1.36~20.86) 0.020 牙齿缺失 2[13, 16] 1 265 2 0.310 固定 4.74(2.71~8.30) < 0.001 重度依赖 4[7, 13-14, 17] 25 284 44 0.150 固定 4.89(4.15~5.75) < 0.001 BI指数 3[7-8, 12] 1 270 95 < 0.001 随机 1.68(0.98~2.88) 0.060 注:BI为巴塞尔指数(Bethel index)。 表 3 各影响因素敏感性分析
Table 3. Sensitivity analysis of each influencing factor
影响因素 固定效应模型 随机效应模型 OR(95% CI) P值 OR(95% CI) P值 高龄 1.24(1.19~1.29) < 0.001 1.27(1.06~1.53) 0.010 性别(男) 1.21(0.94~1.55) 0.130 1.11(0.54~2.31) 0.770 进食时间(长) 3.31(1.94~5.65) < 0.001 3.31(1.94~5.65) < 0.001 进食量(少) 1.88(1.52~2.31) < 0.001 2.04(1.22~3.41) 0.007 协助进食 3.15(2.19~4.54) < 0.001 3.15(2.19~4.54) < 0.001 中重度认知障碍 1.98(1.67~2.36) < 0.001 1.98(1.67~2.36) < 0.001 脑血管疾病 6.04(4.31~8.46) < 0.001 8.16(1.10~60.26) 0.040 心血管疾病 4.08(2.41~6.89) < 0.001 4.08(2.41~6.89) < 0.001 肺炎病史 4.08(2.18~7.66) < 0.001 4.08(2.18~7.66) < 0.001 BMI(低) 1.28(1.13~1.46) < 0.001 1.74(0.80~3.75) 0.160 咀嚼困难 9.25(7.98~10.72) < 0.001 5.33(1.36~20.86) 0.020 牙齿缺失 4.74(2.71~8.30) < 0.001 4.77(2.67~8.49) < 0.001 重度依赖 4.89(4.15~5.75) < 0.001 4.67(3.34~6.52) < 0.001 BI指数 0.98(0.97~0.99) < 0.001 1.68(0.98~2.88) 0.060 -
[1] THIYAGALINGAM S, KULINSKI A E, THORSTEINSDOTTIR B, et al. Dysphagia in older adults[J]. Mayo Clin Proc, 2021, 96(2): 488-497. doi: 10.1016/j.mayocp.2020.08.001 [2] DOAN T N, HO W C, WANG L H, et al. Prevalence and methods for assessment of oropharyngeal dysphagia in older adults: a systematic review and meta-analysis[J]. J Clin Med, 2022, 11(9): 2605. DOI: 10.3390/jcm11092605. [3] BOSCH G, COMAS M, DOMINGO L, et al. Dysphagia in hospitalized patients: prevalence, related factors and impact on aspiration pneumonia and mortality[J]. Eur J Clin Invest, 2023, 53(4): e13930. DOI: 10.1111/eci.13930. [4] KO D, OH J, JOO S, et al. Dietary habits, food product selection attributes, nutritional status, and depression in middle-aged and older adults with dysphagia[J]. Nutrients, 2022, 14(19): 4045. DOI: 10.3390/nu14194045. [5] YANG R Y, YANG A Y, CHEN Y C, et al. Association between dysphagia and frailty in older adults: a systematic review and meta-analysis[J]. Nutrients, 2022, 14(9): 1812. DOI: 10.3390/nu14091812. [6] 曾宪涛, 刘慧, 陈曦, 等. Meta分析系列之四: 观察性研究的质量评价工具[J]. 中国循证心血管医学杂志, 2012, 4(4): 297-299. doi: 10.3969/j.1674-4055.2012.04.004ZENG X T, LIU H, CHEN X, et al. Meta-analysis series 4: quality assessment tools for observational studies[J]. Chinese Journal of Evidence-Based Cardiovascular Medicine, 2012, 4(4): 297-299. doi: 10.3969/j.1674-4055.2012.04.004 [7] PARK Y H, HAN H R, OH B M, et al. Prevalence and associated factors of dysphagia in nursing home residents[J]. Geriatr Nurs, 2013, 34(3): 212-217. doi: 10.1016/j.gerinurse.2013.02.014 [8] MONCAYO-HERNANDEZ B A, HERRERA-GUERRERO J A, VINAZCO S, et al. Sarcopenic dysphagia in institutionalised older adults[J]. Endocrinol Diabetes Nutr (Engl Ed), 2021, 68(9): 602-611. [9] XAVIER J S, GOIS A C B, COSTA LIMA K, et al. Swallowing disorders and associated factors in older adults living in nursing homes[J]. Eur Arch Otorhinolaryngol, 2022, 279(7): 3733-3740. doi: 10.1007/s00405-022-07355-1 [10] OKABE Y, TAKEUCHI K, IZUMI M, et al. Posterior teeth occlusion and dysphagia risk in older nursing home residents: a cross-sectional observational study[J]. J Oral Rehabil, 2017, 44(2): 89-95. doi: 10.1111/joor.12472 [11] HAGGLUND P, GUSTAFSSON M, LOVHEIM H. Oropharyngeal dysphagia and associated factors among individuals living in nursing homes in northern Sweden in 2007 and 2013[J]. BMC Geriatr, 2022, 22(1): 421. DOI: 10.1186/s12877-022-03114-3. [12] CHEN S, CUI Y, DING Y, et al. Prevalence and risk factors of dysphagia among nursing home residents in eastern China: a cross-sectional study[J]. BMC Geriatr, 2020, 20(1): 352. doi: 10.1186/s12877-020-01752-z [13] PU D, MURRY T, WONG M, et al. Indicators of dysphagia in aged care facilities[J]. J Speech Lang Hear Res, 2017, 60(9): 2416-2426. doi: 10.1044/2017_JSLHR-S-17-0028 [14] 刘金枚, 李航, 彭杨, 等. 医养结合型养老机构老年人吞咽障碍发生现状及影响因素分析[J]. 中华现代护理杂志, 2023, 29(2): 227-232. doi: 10.3760/cma.j.cn115682-20220420-01954LIU J M, LI H, PENG Y, et al. Status quo and influencing factors of dysphagia in elderly people in integrated medical and nursing service institution for the aged[J]. Chinese Journal of Modern Nursing, 2023, 29(2): 227-232. doi: 10.3760/cma.j.cn115682-20220420-01954 [15] 高薇薇, 张晓晓, 白银婷. 宁波市养老院老年人吞咽功能障碍调查[J]. 中国康复理论与实践, 2019, 25(7): 761-765.GAO W W, ZHANG X X, BAI Y T. Swallowing dysfunction for old people in nursing homes in Ningbo[J]. Chinese Journal of Rehabilitation Theory and Practice, 2019, 25(7): 761-765. [16] 陈丽丽, 李红, 林榕, 等. 老年痴呆患者吞咽困难状况及危险因素分析[J]. 护理学杂志, 2014, 29(21): 24-26. doi: 10.3870/hlxzz.2014.21.024CHEN L L, LI H, LIN R, et al. Prevalence and associated factors of dysphagia in elderly patients with dementia[J]. Journal of Nursing Science, 2014, 29(21): 24-26. doi: 10.3870/hlxzz.2014.21.024 [17] STREICHER M, WIRTH R, SCHINDLER K, et al. Dysphagia in nursing homes-results from the NutritionDay Project[J]. J Am Med Dir Assoc, 2018, 19(2): 141-147. doi: 10.1016/j.jamda.2017.08.015 [18] NOGUEIRA D, REIS E. Swallowing disorders in nursing home residents: how can the problem be explained?[J]. Clin Interv Aging, 2013, 8: 221-227. [19] HOLLINGHURST J, SMITHARD D G. Identifying dysphagia and demographic associations in older adults using electronic health records: a national longitudinal observational study in Wales (United Kingdom) 2008-2018[J]. Dysphagia, 2022, 37(6): 1612-1622. doi: 10.1007/s00455-022-10425-5 [20] PICCA A, LOZANOSKA-OCHSER B, CALVANI R, et al. Inflammatory, mitochondrial, and senescence-related markers: underlying biological pathways of muscle aging and new therapeutic targets[J]. Exp Gerontol, 2023, 178: 112204. DOI: 10.1016/j.exger.2023.112204. [21] JING X, YANG M, LIU Y, et al. Associations of trunk muscle mass and muscle quality Indicators with self-reported dysphagia in older inpatients[J]. Dysphagia, 2023, 38(1): 415-424. doi: 10.1007/s00455-022-10480-y [22] CHRISTMAS C, ROGUS-PULIA N. Swallowing disorders in the older population[J]. J Am Geriatr Soc, 2019, 67(12): 2643-2649. doi: 10.1111/jgs.16137 [23] 林伟权, 孙敏英, 刘览, 等. 广州市社区老年人慢性病共病与营养状况相关性研究[J]. 中华全科医学, 2022, 20(11): 1870-1873. doi: 10.16766/j.cnki.issn.1674-4152.002723LIN W Q, SUN M Y, LIU L, et al. Study on the relationship between multimorbidity and nutritional status among the community-dwelling elderly people in Guangzhou[J]. Chinese Journal of General Practice, 2022, 20(11): 1870-1873. doi: 10.16766/j.cnki.issn.1674-4152.002723 [24] WATANABE Y, OKADA K, KONDO M, et al. Oral health for achieving longevity[J]. Geriatr Gerontol Int, 2020, 20(6): 526-538. doi: 10.1111/ggi.13921 [25] TRAN T P, NGUYEN L T, HIROSE K, et al. Malnutrition is associated with dysphagia in Vietnamese older adult inpatients[J]. Asia Pac J Clin Nutr, 2021, 30(4): 588-594. [26] DEHAGHANI S E, DOOSTI A, ZARE M. Association between swallowing disorders and cognitive disorders in adults: a systematic review and meta-analysis[J]. Psychogeriatrics, 2021, 21(4): 668-674. doi: 10.1111/psyg.12704 [27] ESTARLICH M, TOLSA C, TRAPERO I, et al. Circadian variations and associated factors in patients with ischaemic heart disease[J]. Int J Environ Res Public Health, 2022, 19(23): 15628. DOI: 10.3390/ijerph192315628. [28] MATSUO H, YOSHIMURA Y, FUJITA S, et al. Incidence of dysphagia and its association with functional recovery and 1-year mortality in hospitalized older patients with heart failure: a prospective cohort study[J]. JPEN J Parenter Enteral Nutr, 2021, 45(2): 372-380. doi: 10.1002/jpen.1845 [29] 江方辉, 应忠明, 施玲玲. 揿针埋针联合吞咽康复训练治疗脑卒中后吞咽障碍的效果观察[J]. 中华全科医学, 2021, 19(3): 483-485. doi: 10.16766/j.cnki.issn.1674-4152.001841JIANG F H, YING Z M, SHI L L. Observation on the effect of pressing needle embedding acupuncture point combined with swallowing rehabilitation training on dysphagia after stroke[J]. Chinese Journal of General Practice, 2021, 19(3): 483-485. doi: 10.16766/j.cnki.issn.1674-4152.001841 [30] YOSHIMATSU Y, MELGAARD D, WESTERGREN A, et al. The diagnosis of aspiration pneumonia in older persons: a systematic review[J]. Eur Geriatr Med, 2022, 13(5): 1071-1080. doi: 10.1007/s41999-022-00689-3 [31] TEZZE C, SANDRI M, TESSARI P. Anabolic resistance in the pathogenesis of sarcopenia in the elderly: role of nutrition and exercise in young and old people[J]. Nutrients, 2023, 15(18): 4073. DOI: 10.3390/nu15184073. [32] ISHII M, NAKAGAWA K, YOSHIMI K, et al. Time spent away from bed to maintain swallowing function in older adults[J]. Gerontology, 2023, 69(1): 37-46. doi: 10.1159/000522499 [33] 余丽丽. 老年患者吞咽障碍风险预测模型的建立[D]. 十堰: 湖北医药学院, 2021.YU L L. Establishment of risk prediction model for dysphagia in elderly patients[D]. Shiyan: Hubei University of Medicine, 2021. [34] NISHIDA T, YAMABE K, HONDA S. Dysphagia is associated with oral, physical, cognitive and psychological frailty in Japanese community-dwelling elderly persons[J]. Gerodontology, 2020, 37(2): 185-190. doi: 10.1111/ger.12455 [35] BANDA K J, CHU H, CHEN R, et al. Prevalence of oropharyngeal dysphagia and risk of pneumonia, malnutrition, and mortality in adults aged 60 years and older: a meta-analysis[J]. Gerontology, 2022, 68(8): 841-853. doi: 10.1159/000520326 -





 下载:
下载: