Establish Nomogram for myocardial damage in emergency sepsis patients based on mitochondrial damage index, and evaluate its predictive efficacy
-
摘要:
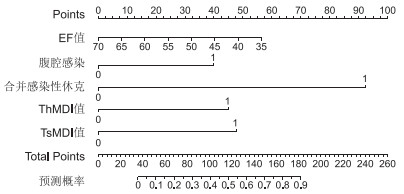
目的 基于线粒体损伤指数(MDI)探究急诊脓毒症患者发生心肌损伤的风险指标,并构建诺莫图预测模型,验证其预测效能。 方法 选取2022年3月—2024年3月于郑州大学附属郑州中心医院确诊并治疗的156例急诊脓毒症患者,根据是否发生心肌损伤分为心肌损伤组(98例)及非心肌损伤组(58例)。入院当天抽取患者外周静脉血,采用流式细胞术检测血清T淋巴细胞亚群和辅助性T细胞(Th)、抑制性T细胞(Ts)的MDI,采用单因素及多因素分析研究影响急诊脓毒症患者心肌损伤的指标,构建诺莫图模型,通过ROC曲线分析诺莫图预测效能。 结果 心肌损伤组患者高血脂、肺部感染、腹腔感染、合并感染性休克、心室舒张早期和心室舒张末期的血流流速(E/A)比值、CD3+、CD4+、CD8+、Th MDI阳性、Ts MDI阳性均高于非心肌损伤组(P<0.05),心室射血分数(EF)低于非心肌损伤组(P<0.05)。腹腔感染、合并感染性休克、EF、Th MDI阳性及Ts MDI阳性是急诊脓毒症患者发生心肌损伤的影响因素。据此构建诺莫图模型,校准曲线显示一致性指数为0.866(95% CI:0.773~0.945),H-L拟合优度检验χ2=6.476(P>0.05),ROC曲线下面积为0.829(95% CI:0.744~0.906),灵敏度、特异度分别为80.70%、72.00%。 结论 腹腔感染、合并感染性休克、EF值、Th MDI阳性及Ts MDI阳性是急诊脓毒症患者发生心肌损伤的影响因素,所构建的诺莫图模型对急诊脓毒症患者发生心肌损伤预测效果良好。 Abstract:Objective The present study investigates the risk index of myocardial damage in patients with emergency sepsis based on mitochondrial damage index (MDI). In addition, the prediction model of Nomograph was constructed to verify its prediction efficiency. Methods A prospective analysis was performed on 156 patients with acute sepsis who were diagnosed and treated in Zhengzhou Central Hospital Affiliated to Zhengzhou University from March 2022 to March 2024, and they were divided into two groups: a myocardial injury group (98 cases) and non-myocardial injury group (58 cases) according to whether myocardial injury occurred. Peripheral venous blood was collected on the day of admission, and the MDI of serum T lymphocyte subsets, helper T cells (Th) and inhibitory T cells (Ts) were detected by flow cytometry. The indicators affecting myocardial injury in patients with emergency sepsis were analyzed by uni-factor and multi-factor analysis, and the prediction efficiency of Nomogram was analyzed by receiver operating characteristic curve (ROC). Results The myocardial injury group exhibited elevated levels of hyperlipidemia, pulmonary infection, abdominal infection, septic shock, E/A, CD3+, CD4+, CD8+, Th MDI positive and Ts MDI positive when compared to the myocardial injury group were higher than those in non-myocardial injury group (P < 0.05), and EF value was found to be lower in the myocardial injury group than that in the non-myocardial injury group (P < 0.05). Peritoneal infection, septic shock, ejection fraction (EF), Th MDI positive and Ts MDI positive are the influential factors for myocardial injury in emergency sepsis patients. The calibration curve demonstrated that the consistency index was 0.866 (95% CI: 0.773-0.945), the H-L goodness-of-fit test (χ2=6.476, P>0.05), and the area under the ROC curve was 0.829 (95% CI: 0.744-0.906). The sensitivity and specificity were found to be 80.70% and 72.00%, respectively. Conclusion Abdominal infection, septic shock, EF, Th MDI positive and Ts MDI positive are the influential factors for myocardial injury in emergency sepsis patients. The Nomograph model established in this study has been shown to be an effective in predicting myocardial injury. -
Key words:
- Emergency sepsis /
- Myocardial injury /
- Mitochondrial damage index /
- Nomogram
-
表 1 2组急诊脓毒症患者一般情况比较
Table 1. Comparison of general conditions between the two groups of patients with acute sepsis
组别 例数 年龄(x±s,岁) 性别[例(%)] BMI (x±s) 饮酒史[例(%)] 吸烟史[例(%)] 基础病史[例(%)] 男性 女性 糖尿病 高血压 高血脂 心肌损伤组 98 52.18±6.34 52(53.06) 46(46.94) 22.68±3.05 45(45.92) 37(37.76) 20(20.41) 41(41.84) 36(36.73) 非心肌损伤组 58 53.10±7.06 33(56.90) 25(43.10) 21.94±3.28 26(44.83) 20(34.48) 11(18.97) 16(27.59) 11(18.97) 统计量 0.839a 0.216b 1.424a 0.017b 0.168b 5.465b 3.191b 5.465b P值 0.403 0.642 0.157 0.895 0.682 0.019 0.740 0.019 组别 例数 病原菌检出率[例(%)] 合并感染性休克[例(%)] 感染部位[例(%)] EF (x±s,%) E/A (x±s) 阳性 阴性 肺部感染 腹腔感染 血流感染 其他感染 心肌损伤组 98 33(33.67) 65(66.33) 78(79.59) 51(52.04) 31(31.63) 14(14.29) 2(2.04) 49.15±4.39 1.28±0.11 非心肌损伤组 58 19(32.76) 39(67.24) 8(13.79) 42(72.41) 5(8.62) 10(17.24) 1(1.72) 56.84±5.81 1.24±0.10 统计量 0.014b 68.770b 6.282b 10.869b 0.245b 0.019b 9.353a 2.269a P值 0.907 <0.001 0.012 <0.001 0.621 0.889 <0.001 0.025 注:a为t值,b为χ2值。 表 2 2组急诊脓毒症患者T淋巴细胞亚群及MDI指标比较
Table 2. Comparison of T lymphocyte subsets and MDI indexes between the two groups of patients with acute sepsis
组别 例数 CD3+ (x±s,%) CD4+ (x±s,%) CD8+ (x±s,%) Th MDI阳性[例(%)] Ts MDI阳性[例(%)] 心肌损伤组 98 75.98±8.26 41.07±5.86 32.69±3.54 62(63.27) 73(74.49) 非心肌损伤组 58 68.54±7.52 37.99±4.71 30.15±3.85 20(34.48) 27(46.55) 统计量 5.618a 3.403a 4.192a 12.106b 12.359b P值 <0.001 <0.001 <0.001 <0.001 <0.001 注:a为t值,b为χ2值。 表 3 变量赋值情况
Table 3. Variable assignment
变量 赋值方法 高血脂 否=0,是=1 肺部感染 否=0,是=1 腹腔感染 否=0,是=1 合并感染性休克 否=0,是=1 EF 以实际值赋值 E/A 以实际值赋值 CD3+ 以实际值赋值 CD4+ 以实际值赋值 CD8+ 以实际值赋值 Th MDI阳性 否=0,是=1 Ts MDI阳性 否=0,是=1 表 4 急诊脓毒症患者发生心肌损伤的logistic回归分析
Table 4. Logistic regression analysis of myocardial injury in patients with acute sepsis
变量 B SE Waldχ2 P值 OR值 95% CI 高血脂 0.527 0.325 2.629 0.115 1.694 1.057~2.331 肺部感染 0.663 0.342 3.758 0.069 1.941 1.270~2.611 腹腔感染 0.798 0.365 4.780 0.047 2.221 1.506~2.936 合并感染性休克 0.965 0.251 14.781 <0.001 2.625 2.324~3.649 EF 1.094 0.338 10.476 <0.001 2.986 2.133~3.117 E/A 0.632 0.294 4.621 0.058 1.881 1.305~2.458 CD3+ 0.615 0.365 2.839 0.095 1.850 1.134~2.565 CD4+ 0.734 0.405 3.285 0.074 2.083 1.290~2.877 CD8+ 0.711 0.418 2.893 0.086 2.036 1.217~2.855 Th MDI阳性 0.735 0.288 6.513 0.025 2.085 1.521~2.650 Ts MDI阳性 0.826 0.276 8.957 0.011 2.284 1.743~2.825 -
[1] FRENCKEN J F, VAN SMEDEN M, VAN DE GROEP K, et al. Etiology of myocardial injury in critically ill patients with sepsis: a cohort study[J]. Ann Am Thorac Soc, 2022, 19(5): 773-780. doi: 10.1513/AnnalsATS.202106-689OC [2] 秦苏徽, 顿士娟. 脓毒症相关凝血功能障碍患者发病及预后危险因素分析[J]. 中华全科医学, 2021, 19(12): 2020-2023. doi: 10.16766/j.cnki.issn.1674-4152.002225QIN S H, DUN S J. Analysis of risk factors for the pathogenesis and prognosis of patients with sepsis-associated coagulopathy[J]. Chinese Journal of General Practice, 2021, 19(12): 2020-2023. doi: 10.16766/j.cnki.issn.1674-4152.002225 [3] LIU C, ZOU Q, TANG H X, et al. Melanin nanoparticles alleviate sepsis-induced myocardial injury by suppressing ferroptosis and inflammation[J]. Bioact Mater, 2022, 24: 313-321. [4] LIU H R, XU C Q, HU Q, et al. Sepsis-induced cardiomyopathy: understanding pathophysiology and clinical implications[J]. Arch Toxicol, 2024. DOI: 10.1007/s00204-024-03916-x. [5] HOLLENBERG S M, SINGER M. Pathophysiology of sepsis-induced cardiomyopathy[J]. Nat Rev Cardiol, 2021, 18(6): 424-434. doi: 10.1038/s41569-020-00492-2 [6] TODOROVIC MARKOVIC M, TODOROVIC MITIC M, IGNJATOVIC A, et al. Mortality in community-acquired sepsis and infections in the Faroe Islands: a prospective observational study[J]. Infect Dis Rep, 2024, 16(3): 448-457. doi: 10.3390/idr16030033 [7] JIANG T, WANG Q, LV J G, et al. Mitochondria-endoplasmic reticulum contacts in sepsis-induced myocardial dysfunction[J]. Front Cell Dev Biol, 2022, 10: 1036225. DOI: 10.3389/fcell.2022.1036225. [8] KUROSHIMA T, KAWAGUCHI S, OKADA M. Current perspectives of mitochondria in sepsis-induced cardiomyopathy[J]. Int J Mol Sci, 2024, 25(9): 4710. DOI: 10.3390/ijms25094710. [9] SRZIĆ I, NESEK ADAM V, TUNJIĆ PEJAK D. Sepsis definition: what's new in the treatment guidelines[J]. Acta Clin Croat, 2022, 61(Suppl 1): 67-72. [10] NASERI A, AKYUZ E, TURGUT K, et al. Sepsis-induced cardiomyopathy in animals: from experimental studies to echocardiography-based clinical research[J]. Can Vet J, 2023, 64(9): 871-877. [11] WU F, ZHANG Y T, TENG F, et al. S100a8/a9 contributes to sepsis-induced cardiomyopathy by activating ERK1/2-Drp1-mediated mitochondrial fission and respiratory dysfunction[J]. Int Immunopharmacol, 2023, 115: 109716. DOI: 10.1016/j.intimp.2023.109716. [12] 张文静, 李晓峰, 孙明明, 等. 线粒体自噬在心肌梗死中的作用及研究进展[J]. 中华全科医学, 2022, 20(7): 1194-1198. doi: 10.16766/j.cnki.issn.1674-4152.002556ZHANG W J, LI X F, SUN M M, et al. Research progress and function of mitophagy in myocardial infarction[J]. Chinese Journal of General Practice, 2022, 20(7): 1194-1198. doi: 10.16766/j.cnki.issn.1674-4152.002556 [13] NI D, LIN X F, DENG C H, et al. Energy metabolism: from physiological changes to targets in sepsis-induced cardiomyopathy[J]. Hellenic J Cardiol, 2024, 80: 96-106. doi: 10.1016/j.hjc.2024.05.010 [14] SONG J Y, FANG X L, ZHOU K X, et al. Sepsis-induced cardiac dysfunction and pathogenetic mechanisms (review)[J]. Mol Med Rep, 2023, 28(6): 227. DOI: 10.3892/mmr.2023.13114. [15] CHEN T T, YE L, ZHU J, et al. Inhibition of pyruvate dehydrogenase kinase 4 attenuates myocardial and mitochondrial injury in sepsis-induced cardiomyopathy[J]. J Infect Dis, 2024, 229(4): 1178-1188. doi: 10.1093/infdis/jiad365 [16] 韩永燕, 杨俊礼, 孟会敏, 等. 血尿素氮/白蛋白比值联合可溶性生长刺激表达基因2蛋白对急诊重症监护病房老年脓毒症患者心肌损伤的预警价值[J]. 中华老年医学杂志, 2024, 43(6): 727-732.HAN Y Y, YANG J L, MENG H M, et al. Early warning value of blood urea nitrogen to albumin ratio combined with soluble growth stimulation expressed gene 2 on sepsis-induced myocardial injury in elderly patients in emergency intensive care unit[J]. Chinese Journal of Geriatrics, 2024, 43(6): 727-732. [17] SINGAM A. Myocardial injury as a harbinger of multi-organ failure in septic shock: a comprehensive review[J]. Cureus, 2024, 16(2): e55021. DOI: 10.7759/cureus.55021. [18] BLIXT P J, NGUYEN M, CHOLLEY B, et al. Association between left ventricular systolic function parameters and myocardial injury, organ failure and mortality in patients with septic shock[J]. Ann Intensive Care, 2024, 14(1): 12. DOI: 10.1186/s13613-023-01235-5. [19] 陆珏秀, 刘先霞, 闫霖. 左室射血分数在急性心肌梗死中应用的研究进展[J]. 临床医学进展, 2023, 13(2): 1203-1208.LU J X, LIU X X, YAN L. Research progress of left ventricular ejection fraction in acute myocardial infarction[J]. Advances in Clinical Medicine, 2023, 13(2): 1203-1208. [20] DE NUNZIO C, GHAHHARI J, LOMBARDO R, et al. Development of a nomogram predicting the probability of stone free rate in patients with ureteral stones eligible for semi-rigid primary laser uretero-litothripsy[J]. World J Urol, 2021, 39(11): 4267-4274. doi: 10.1007/s00345-021-03768-5 -





 下载:
下载: