Comparison of the predictive value of the TyG index and related indices for lean non-alcoholic fatty liver disease
-
摘要:
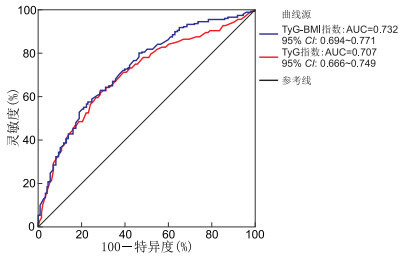
目的 探讨甘油三酯-葡萄糖指数(TyG指数)反映胰岛素抵抗的能力,与非酒精性脂肪肝病(NAFLD)的关联,分析其和相关指数对瘦型非酒精性脂肪肝病的预测效能。 方法 选取2023年7—9月于皖南医学院第一附属医院体检中心进行体检的1 343例体检者,使用腹部超声诊断NAFLD,分为非NAFLD组(1 099例)和NAFLD(244例),对比2组间指标差异。采用logistic回归分析探讨瘦型非酒精性脂肪肝的危险因素,绘制TyG指数及相关指数的ROC曲线,评估指标对瘦型NAFLD的预测价值。 结果 TyG指数、TyG-BMI指数是瘦型NAFLD发病的独立影响因素(P<0.05)。在总体及性别分组的ROC分析结果中显示,TyG-BMI指数的预测价值最高,曲线下面积(AUC)在总体、男性、女性分别为0.747(95% CI: 0.713~0.782)、0.725(95% CI: 0.672~0.779)、0.748(95% CI: 0.700~0.796)。 结论 TyG指数和TyG-BMI指数是NAFLD的独立影响因素,均具有较好的预测价值,其中TyG-BMI指数的预测价值更高。 -
关键词:
- 瘦型非酒精性脂肪肝病 /
- 甘油三酯-葡萄糖指数 /
- 相关指标 /
- 预测效能
Abstract:Objective To investigate the utility of the triglyceride-glucose index (TyG index) as a surrogate marker of insulin resistance, examine its association with non-alcoholic fatty liver disease (NAFLD), and assess its predictive efficacy, along with related indices, for lean NAFLD. Methods A total of 1 343 individuals who underwent health examinations at the Medical Examination Center of the First Affiliated Hospital of Wannan Medical College from June to August 2023 were selected. NAFLD was diagnosed using abdominal ultrasound, and participants were categorized into a non-NAFLD group (1 099 cases) and a NAFLD group (244 cases). Clinical indices between the two groups were compared. Logistic regression was used to explore the risk factors for lean NAFLD. Receiver operating characteristic (ROC) curve was generated to assess the predictive value of the TyG index and related indices. Results Both the TyG index and TyG-BMI index were independent risk factors for the development of lean NAFLD (P < 0.05). The ROC curve results for the total population and gender subgroups showed that the TyG-BMI index had the highest predictive value, with an area under the curve (AUC) of 0.747 (95% CI: 0.713-0.782) in the total population, 0.725 (95% CI: 0.672-0.779) in males, and 0.748 (95% CI: 0.700-0.796) in females. Conclusion Both the TyG index and TyG-BMI index are independent risk factors for NAFLD, showing good predictive ability, with the TyG-BMI index exhibiting superior predictive performance. -
Key words:
- Lean non-alcoholic fatty liver disease /
- TyG index /
- Correlation index /
- Predictive value
-
表 1 非NAFLD与NAFLD组患者一般资料比较
Table 1. Comparison of baseline characteristics between the non-NAFLD and NAFLD groups
组别 例数 性别[例(%)] 年龄[M(P25, P75),岁] 吸烟史[例(%)] 饮酒史[例(%)] 高血压[例(%)] 男性 女性 无 有 无 有 无 有 非NAFLD 1 099 341(31.0) 758(69.0) 54(49.0, 64.0) 985(89.6) 114(10.4) 968(88.1) 131(11.9) 872(79.3) 227(20.7) NAFLD 244 115(47.1) 129(52.9) 57(51.3, 66.0) 211(86.5) 33(13.5) 193(79.1) 51(20.9) 160(65.6) 84(34.4) 统计量 23.008a -3.433b 2.034a 13.746a 21.276a P值 <0.001 0.001 0.154 <0.001 <0.001 注:a为χ2值,b为Z值。 表 2 非NAFLD与NAFLD组患者临床资料比较[M(P25, P75)]
Table 2. Comparison of clinical data between the non-NAFLD and NAFLD groups[M(P25, P75)]
组别 例数 BMI 空腹血糖(mmol/L) 总胆固醇(mmol/L) 甘油三酯(mmol/L) 高密度脂蛋白(mmol/L) 低密度脂蛋白(mmol/L) 非NAFLD 1 099 21.07(20.03, 22.07) 4.91(4.58, 5.31) 5.06(4.46, 5.69) 1.10(0.80, 1.45) 1.65(1.42, 1.87) 2.81(2.36, 3.35) NAFLD 244 21.93(21.08, 22.58) 5.29(4.90, 6.00) 5.15(4.55, 5.83) 1.64(1.09, 2.23) 1.45(1.29, 1.67) 3.00(2.51, 3.54) Z值 -7.852 -8.790 -1.486 -9.815 -6.691 -2.752 P值 <0.001 <0.001 0.137 <0.001 <0.001 0.006 组别 例数 TyG指数 TyG-BMI指数 TG/HDL-C指数 TC/HDL-C指数 LDL-C/HDL-C指数 非NAFLD 1 099 8.38(8.05, 8.68) 175.87(164.72, 187.40) 0.66(0.44, 0.94) 3.03(2.63, 3.55) 1.72(1.38, 2.13) NAFLD 244 8.85(8.46, 9.29) 193.50(179.96, 204.27) 1.13(0.69, 1.63) 3.49(2.92, 4.08) 2.01(1.64, 2.47) Z值 -10.996 -12.110 -9.933 -7.268 -6.527 P值 <0.001 <0.001 <0.001 <0.001 <0.001 表 3 发生NAFLD影响因素的多因素logistic回归分析
Table 3. Multivariable logistic regression analysis
项目 B SE Waldχ2 P值 OR(95% CI) TyG指数 0.712 0.288 6.098 0.014 2.038(1.158~3.587) TyG-BMI指数 0.039 0.008 26.036 <0.001 1.040(1.024~1.055) TG/HDL-C指数 -0.101 0.159 0.402 0.526 0.904(0.663~1.234) TC/HDL-C指数 -0.491 0.334 2.157 0.142 0.612(0.318~1.178) LDL-C/HDL-C指数 0.671 0.382 3.091 0.079 1.956(0.926~4.133) 表 4 TyG指数及相关指数预测与NAFLD比较
Table 4. Comparison of the predictive performance of the TyG index and related indices for NAFLD
预测指标 AUC 95% CI 灵敏度 特异度 最佳临界值 P值 总体 TyG指数 0.725 0.687~0.762 0.619 0.748 8.671 <0.001 TyG-BMI指数 0.747 0.713~0.782 0.697 0.689 184.160 <0.001 男性 TyG指数 0.686 0.627~0.746 0.687 0.628 8.602 <0.001 TyG-BMI指数 0.725 0.672~0.779 0.609 0.748 191.053 <0.001 女性 TyG指数 0.744 0.695~0.793 0.636 0.772 8.671 <0.001 TyG-BMI指数 0.748 0.700~0.796 0.674 0.735 184.687 <0.001 -
[1] GUO X Y, YIN X Z, LIU Z J, et al. Non-alcoholic fatty liver disease (NAFLD) pathogenesis and natural products for prevention and treatment[J]. Int J Mol Sci, 2022, 23(24): 15489. DOI: 10.3390/ijms232415489. [2] KUCHAY M S, MARTÍNEZ-MONTORO J I, CHOUDHARY N S, et al. Non-Alcoholic fatty liver disease in lean and non-obese individuals: current and future challenges[J]. Biomedicines, 2021, 9(10): 1346. DOI: 10.3390/biomedicines9101346. [3] KIM Y, HAN E, LEE J S, et al. Cardiovascular risk is elevated in lean subjects with nonalcoholic fatty liver disease[J]. Gut Liver, 2022, 16(2): 290-299. doi: 10.5009/gnl210084 [4] WIJARNPREECHA K, LI F, LUNDIN S K, et al. Higher mortality among lean patients with non-alcoholic fatty liver disease despite fewer metabolic comorbidities[J]. Aliment Pharmacol Ther, 2023, 57(9): 1014-1027. doi: 10.1111/apt.17424 [5] NABI O, LAPIDUS N, BOURSIER J, et al. Lean individuals with NAFLD have more severe liver disease and poorer clinical outcomes (NASH-CO Study)[J]. Hepatology, 2023, 78(1): 272-283. doi: 10.1097/HEP.0000000000000329 [6] PATEL A H, PEDDU D, AMIN S, et al. Nonalcoholic fatty liver disease in lean/nonobese and obese individuals: a comprehensive review on prevalence, pathogenesis, clinical outcomes, and treatment[J]. J Clin Transl Hepatol, 2023, 11(2): 502-515. [7] SON D H, LEE H S, LEE Y J, et al. Comparison of triglyceride-glucose index and HOMA-IR for predicting prevalence and incidence of metabolic syndrome[J]. Nutr Metab Cardiovasc Dis, 2022, 32(3): 596-604. doi: 10.1016/j.numecd.2021.11.017 [8] MUHAMMAD I F, BAO X, NILSSON P M, et al. Triglyceride-glucose (TyG) index is a predictor of arterial stiffness, incidence of diabetes, cardiovascular disease, and all-cause and cardiovascular mortality: a longitudinal two-cohort analysis[J]. Front Cardiovasc Med, 2022, 9: 1035105. DOI: 10.3389/fcvm.2022.1035105. [9] XUE Y, XU J H, LI M, et al. Potential screening indicators for early diagnosis of NAFLD/MAFLD and liver fibrosis: triglyceride glucose index-related parameters[J]. Front Endocrinol, 2022, 13: 951689. DOI: 10.3389/fendo.2022.951689. [10] LIU H S, CHEN J F, QIN Q, et al. Association between TyG index trajectory and new-onset lean NAFLD: a longitudinal study[J]. Front Endocrinol, 2024, 15: 1321922. DOI: 10.3389/fendo.2024.1321922. [11] 中华医学会肝病学分会. 代谢相关(非酒精性)脂肪性肝病防治指南(2024年版)[J]. 实用肝脏病杂志, 2024, 27(4): 494-510.Chinese Society of Hepatology, Chinese Medical Association. Guidelines for the prevention and treatment of metabolic dysfunction-associated (non-alcoholic) fatty liver disease(Version 2024)[J]. Journal Of Practical Hepatology, 2024, 27(4): 494-510. [12] 左广民, 彭魁, 李勉, 等. 上海社区中老年人群脂肪肝指数与微量白蛋白尿的相关性研究[J]. 诊断学理论与实践, 2020, 19(6): 605-609.ZUO G M, PENG K, LI M, et al. The association between fatty liver index and microalbuminuria in middle-aged and elderly population in Shanghai[J]. Journal of Diagnostics Concepts & Practice, 2020, 19(6): 605-609. [13] RIAZI K, AZHARI H, CHARETTE J H, et al. The prevalence and incidence of NAFLD worldwide: a systematic review and meta-analysis[J]. Lancet Gastroenterol Hepatol, 2022, 7(9): 851-861. doi: 10.1016/S2468-1253(22)00165-0 [14] SHAUNAK M, BYRNE C D, DAVIS N, et al. Non-alcoholic fatty liver disease and childhood obesity[J]. Arch Dis Child, 2021, 106(1): 3-8. doi: 10.1136/archdischild-2019-318063 [15] QUEK J, CHAN K E, WONG Z Y, et al. Global prevalence of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in the overweight and obese population: a systematic review and meta-analysis[J]. Lancet Gastroenterol Hepatol, 2023, 8(1): 20-30. doi: 10.1016/S2468-1253(22)00317-X [16] DIKAIAKOU E, VLACHOPAPADOPOULOU E A, PASCHOU S A, et al. Triglycerides-glucose (TyG) index is a sensitive marker of insulin resistance in Greek children and adolescents[J]. Endocrine, 2020, 70(1): 58-64. doi: 10.1007/s12020-020-02374-6 [17] CHEN Q L, HU P P, HOU X X, et al. Association between triglyceride-glucose related indices and mortality among individuals with non-alcoholic fatty liver disease or metabolic dysfunction-associated steatotic liver disease[J]. Cardiovasc Diabetol, 2024, 23(1): 232. DOI: 10.1186/s12933-024-02343-7. [18] 白敏, 黄烈平, 朱蓓, 等. 瘦素水平在肥胖儿童胰岛素抵抗与非酒精性脂肪肝间的中介效应[J]. 中华全科医学, 2023, 21(12): 2086-2088, 2105. doi: 10.16766/j.cnki.issn.1674-4152.003296BAI M, HUANG L P, ZHU B, et al. Mediating effect of leptin levels between insulin resistance and nonalcoholic fatty liver disease in obese children[J]. Chinese Journal of General Practice, 2023, 21(12): 2086-2088, 2105. doi: 10.16766/j.cnki.issn.1674-4152.003296 [19] KUANG M B, SHENG G T, HU C, et al. The value of combining the simple anthropometric obesity parameters, body mass index (BMI) and a body shape index (ABSI), to assess the risk of non-alcoholic fatty liver disease[J]. Lipids Health Dis, 2022, 21(1): 104. DOI: 10.1186/s12944-022-01717-8. -





 下载:
下载: