Analysis of comorbidities and survival of patients with advanced lung squamous cell carcinoma
-
摘要:
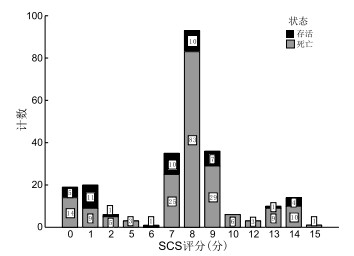
目的 分析晚期肺鳞癌患者的临床特征和共病患病情况,探讨晚期肺癌患者预后的影响因素。 方法 回顾性分析2017年1月—2021年12月海军军医大学第一附属医院呼吸内科收治的晚期肺鳞癌患者的临床资料,随访截止时间为2023年8月31日。统计分析患者的性别、年龄、症状、吸烟情况、癌症分期、治疗情况以及生存期等相关指标,采用简化合并症评分(SCS)量化评估共病情况。采用Kaplan-Meier法绘制患者总生存期(OS)生存曲线,以单因素和多因素Cox回归分析共病对晚期肺鳞癌OS的预测能力,并分析影响晚期肺鳞癌预后的因素。 结果 共纳入247例患者,平均年龄为65.57岁,男性217例,女性30例,193例患者有吸烟史,死亡197例。患者中位SCS评分为8分(0~15分),不同SCS评分组患者生存期差异有统计学意义(P<0.05)。单因素分析显示,性别、吸烟史、纤维蛋白原、PS评分、免疫治疗、SCS评分、慢性肺部疾病均为OS的影响因素(P<0.05)。多因素Cox回归分析显示,吸烟史、纤维蛋白原、PS评分、免疫治疗、SCS评分、慢性肺部疾病是晚期肺鳞癌患者OS的独立影响因素。 结论 简化合并症评分、慢性肺部疾病是晚期肺鳞癌患者OS的独立影响因素。 Abstract:Objective To analyze the clinical characteristics and comorbidities of patients with advanced lung squamous cell carcinoma and to explore the prognostic factors of patients with advanced lung cancer. Methods Clinical data of patients with advanced lung squamous cell carcinoma admitted to the Department of Respiratory Medicine from January 2017 to December 2021 were retrospectively analyzed, with follow-up completed in August 2023. Variables including gender, age, symptoms, smoking status, cancer stage, treatment status, and survival time of patients were statistically analyzed. The simplified comorbidity score (SCS) was used to quantitatively evaluate comorbidities. Kaplan-meier method was used to draw the overall survival (OS) survival curve of patients, and univariate and multivariate Cox regression analyses were used to analyze the predictive ability of OS and to identify prognostic factors in patients with advanced lung squamous cell carcinoma. Results A total of 247 patients were included, with an average age of 65.57 years, 217 cases were male, 30 cases were female, 193 cases had a smoking history, and 197 died during follow-up. In this study, the median score of SCS was 8 points (range 0-15), and significant differences in survival were observed among groups with different SCS assessments (P < 0.05). Univariate analysis showed that gender, smoking history, fibrinogen, PS score, immunotherapy, SCS score, and chronic lung disease were influencing factors of OS (P < 0.05). Multivariate Cox regression analysis showed that smoking history, fibrinogen, PS score, immunotherapy, SCS score, and chronic lung disease were independent factors affecting OS in patients with advanced lung squamous cell carcinoma. Conclusion The simplified comorbidity score and the presence of chronic lung disease are independent risk factors for OS in patients with advanced lung squamous cell carcinoma. -
表 1 SCS评分量表内容
Table 1. Simplified Comorbidities Score (SCS) scale
评分 共病 1分 嗜酒(男性≥80 g/d, 女性≥40 g/d);心脑血管疾病(心力衰竭、冠状动脉疾病、严重的心脏瓣膜病、脑血管病、高血压病、外周血管疾病);肿瘤(不包括皮肤基底癌及宫颈原位癌);呼吸系统疾病(结核病史、胸腔积液或肺炎史、哮喘、肺栓塞、慢性呼吸衰竭、慢性阻塞性肺疾病) 4分 肾功能不全(采用Cockcroft公式计算肌酐清除率≤60 mL/min) 5分 糖尿病 7分 吸烟(一生中至少吸烟≥100支) 表 2 晚期肺鳞癌患者OS的影响因素分析
Table 2. Analysis of factors influencing OS in patients with advanced lung squamous cell carcinoma
变量 单因素分析 多因素分析 HR值 95% CI Z值 P值 HR值 95% CI P值 男性 2.362 1.464~3.811 3.524 <0.001 1.019 0.530~1.961 0.954 诊断时年龄(岁) 51~60 1.103 0.567~2.147 0.289 0.773 61~70 1.282 0.681~2.415 0.770 0.441 ≥71 1.421 0.751~2.691 1.079 0.280 BMI 18~24 0.835 0.460~1.514 -0.594 0.552 >24 0.829 0.446~1.542 -0.592 0.554 有吸烟史 3.005 2.047~4.413 5.615 <0.001 2.047 1.055~3.974 0.034 白蛋白≥40 g/L 0.961 0.708~1.305 -0.253 0.801 纤维蛋白原>4 g/L 1.472 1.081~2.006 2.451 0.014 1.690 1.212~2.355 0.002 肿瘤分期Ⅳ期 1.163 0.873~1.550 1.031 0.303 PS评分≥2分 1.804 1.146~2.840 2.547 0.011 1.706 1.055~2.759 0.030 治疗方案 化疗 0.647 0.382~1.096 -1.619 0.105 放疗 0.783 0.589~1.042 -1.678 0.093 靶向治疗 0.951 0.689~1.312 -0.306 0.759 免疫治疗 0.726 0.547~0.964 -2.211 0.027 0.673 0.496~0.912 0.011 共病 心肌梗死 1.026 0.505~2.085 0.070 0.944 心力衰竭 1.980 0.276~14.201 0.680 0.497 周围血管疾病 1.962 0.625~6.155 1.155 0.248 脑血管疾病 0.548 0.077~3.924 -0.599 0.549 慢性肺部疾病 2.781 1.995~3.877 6.036 <0.001 1.758 1.028~3.005 0.039 结缔组织病 <0.001 <0.001~null -0.009 0.993 中重度肝病 1.043 0.333~3.273 0.073 0.942 酗酒 1.917 0.939~3.914 1.788 0.074 心脑血管疾病 0.893 0.658~1.211 -0.730 0.465 其他肿瘤 1.558 0.386~6.286 0.623 0.533 糖尿病 1.315 0.891~1.942 1.379 0.168 SCS评分(分) 8~9 2.922 2.092~4.082 6.288 <0.001 1.579 0.808~3.086 0.182 ≥10 4.186 2.641~6.635 6.091 <0.001 2.425 1.147~5.128 0.020 注:由于在患有结缔组织病的患者组中未观察到死亡事件(完全分离),无法计算有效的HR值及95% CI;各变量赋值方法如下,女性=0,男性=1;诊断时年龄<50岁=0,51~60岁=1,61~70岁=2,≥71岁=3;BMI<18=0,18~24=1,>24=2;无吸烟史=0,有=1;白蛋白<40 g/L=0,≥40 g/L=1;纤维蛋白原≤40 g/L=0,>40 g/L=1;肿瘤分期为Ⅲ期=0,Ⅳ期=1;PS评分<2分=0,≥2分=1;治疗方案,未接受该治疗=0,接受该治疗=1;共病,无该共病=0,有该共病=1;SCS评分≤7分=0,8~9分=1,≥10分=2。性别以女性为参照;诊断时年龄以≤50岁为参照;BMI以<18为参照;吸烟史以无为参照;白蛋白以<40 g/L为参照;纤维蛋白原以≤4 g/L为参照;肿瘤分期以Ⅲ期为参照;PS评分以<2分为参照;治疗方案以未接受该治疗为参照;共病以无该共病为参照;SCS评分以0~7分为参照。 -
[1] SIEGEL R L, MILLER K D, FUCHS H E, et al. Cancer statistics, 2022[J]. CA Cancer J Clin, 2022, 72(1): 7-33. [2] CHENG Z, CHEN L Z, DONG X F. Long-term response to first-line treatment with sintilimab plus chemotherapy in a patient with advanced lung squamous cell carcinoma: a case report[J]. Asian J Surg, 2024. DOI: 10.1016/j.asjsur.2024.10.181. [3] YASUNORI M, SHIGERU T, TOSHIHIRO M, et al. Multicenter, retrospective study to evaluate necitumumab plus cisplatin and gemcitabine after immune checkpoint inhibitors in advanced squamous cell lung cancer in Japan: the NINJA study[J]. JTO Clin Res Rep, 2023, 4(12): 100593. DOI: 10.1016/j.jtocrr.2023.100593. [4] ANDREAS M N, BÖHMER D, PRATSCHKE J, et al. Advanced lung cancer patient benefits from minimally invasive costal resection and reconstruction: an effective palliative approach for costal metastasis[J]. J Cardiothorac Surg, 2023, 18(1): 310. DOI: 10.1186/s13019-023-02422-y. [5] 中华医学会肿瘤学分会, 中华医学会杂志社. 中华医学会肿瘤学分会肺癌临床诊疗指南(2021版)[J]. 中华肿瘤杂志, 2021, 43(6): 591-621.Oncology Society of Chinese Medical Association, Chinese Medical Association Publishing House. Oncology Society of Chinese Medical Association guideline for clinical diagnosis and treatment of lung cancer (2021 edition)[J]. Chinese Journal of Oncology, 2021, 43(6): 591-621. [6] SHIGERU T, HIROSHIGE Y, EISAKU M, et al. MO57-5 multicenter retrospective study to evaluate necitumumab plus CDDP/GEM after ICIs in advanced squamous-cell lung cancer in Japan (NINJA study)[J]. Ann Oncol, 2023, 34(S3): S1432. DOI: 10.1016/j.annonc.2023.09.297. [7] GAO X F, WANG Z L, LIU J, et al. Impact of COPD pulmonary structural remodeling on the prognosis of patients with advanced lung squamous cell carcinoma[J]. Heliyon, 2023, 9(11): e22042. DOI: org/ 10.1016/j.heliyon.2023.e22042. [8] JIANG M L, SUN J Y, HU C L, et al. A tumor cornification and immune-infiltration-based scheme for anti-PD-1 plus chemotherapy response in advanced squamous cell lung carcinoma[J]. Med, 2025, 6(2): 100516. DOI: 10.1016/j.medj.2024.09.005. [9] YOSHIOKA H, MORI K, ISHIKAWA N, et al. 1357P Multicenter phase Ⅱ study of cisplatin and gemcitabine plus necitumumab in patients with unresectable, advanced lung squamous cell carcinoma who have progressed on orafter initial treatment with immune checkpoint inhibitors plus platinum-based chemotherapy: WJOG14120L NESSIE study[J]. Ann Oncol, 2024, 35(S2): S855-S856. [10] DELMONTE A, BONANNO L, LANDI L, et al. EP08.01-030 nivolumab+ipilimumab vs platinum-based CT+nivolumab in advanced lung squamous-cell carcinoma: the randomized SQUINT trial[J]. J Thorac Oncol, 2022, 17(9S): S351. DOI: 10.1016/j.jtho.2022.07.602. [11] SANTOS E S, RODRIGUEZ E. Treatment considerations for patients with advanced squamous cell carcinoma of the lung: a plain language summary[J]. Lung Cancer Manag, 2022, 11(3): LMT56. DOI: 10.2217/lmt-2022-0017. [12] KOZONO D, HUA X, WU C M, et al. Lung-MAP next generation sequencing analysis of advanced squamous cell lung cancers (SWOG S1400)[J]. J Thorac Oncol, 2024, 19(12): 1618-1629. doi: 10.1016/j.jtho.2024.07.024 [13] MEDIA A S, PERSSON M, TAJHIZI N, et al. Chronic obstructive pulmonary disease and comorbidities ' influence on mortality in non-small cell lung cancer patients[J]. Acta Oncol, 2019, 58(8): 1102-1106. doi: 10.1080/0284186X.2019.1612942 [14] ZHAI R H, YU X J, SHAFER A, et al. The impact of coexisting COPD on survival of patients with early-stage non-small cell lung cancer undergoing surgical resection[J]. Chest, 2014, 145(2): 346-353. doi: 10.1378/chest.13-1176 [15] YUSUKE T, KAZUHITO F, AKIKAZU K, et al. Left upper lobectomy with combined distal aortic arch and left subclavian artery resection after neoadjuvant chemoradiotherapy for locally advanced lung squamous cell carcinoma[J]. Respirol Case Rep, 2022, 10(8): e0994. DOI: 10.1002/rcr2.994. [16] IACHINA M, JAKOBSEN E, MØLLER H, et al. The effect of different comorbidities on survival of non-small cells lung cancer patients[J]. Lung, 2015, 193(2): 291-297. doi: 10.1007/s00408-014-9675-5 [17] 刘允, 刘莹, 刘佳慧, 等. 阿法替尼二线治疗晚期肺鳞癌患者的效果观察[J]. 中华全科医学, 2024, 22(9): 1491-1495, 1499. doi: 10.16766/j.cnki.issn.1674-4152.003666LIU Y, LIU Y, LIU J H, et al. Clinical efficacy of afatinib in second-line treatment of advanced squamous cell carcinoma of the lung[J]. Chinese Journal of General Practice, 2024, 22(9): 1491-1499. doi: 10.16766/j.cnki.issn.1674-4152.003666 [18] SCHREUDER A, JACOBS C, GALLARDO E L, et al. Predicting all-cause and lung cancer mortality using emphysema score progression rate between baseline and follow-up chest CT images: a comparison of risk model performances[J]. PLoS One, 2019, 14(2): e0212756. DOI: 10.1371/journal.pone.0212756. [19] AJIMIZU H, OZASA H, SATO S, et al. Survival impact of treatment for chronic obstructive pulmonary disease in patients with advanced non-small-cell lung cancer[J]. Sci Rep, 2021, 11(1): 23677. DOI: 10.1038/s41598-021-03139-5. [20] JO H, PARK S, KIM N E, et al. Impact of COPD treatment on survival in patients with advanced non-small cell lung cancer[J]. J Clin Med, 2022, 11(9): 2391. DOI: 10.3390/jcm11092391. [21] KASEDA K, HISHIDA T, MASAI K, et al. Clinicopathological and prognostic features of operable non-small cell lung cancer patients with diabetes mellitus[J]. J Surg Oncol, 2021, 123(1): 332-341. doi: 10.1002/jso.26243 [22] JACOBI O, LANDMAN Y, REINHORN D, et al. The relationship of diabetes mellitus to efficacy of immune checkpoint inhibitors in patients with advanced non-small cell lung cancer[J]. Oncology, 2021, 99(9): 555-561. doi: 10.1159/000516671 [23] OSAWA K, BESSHO A, FUKE S, et al. Coronary artery calcification scoring system based on the coronary artery calcium data and reporting system (CAC-DRS) predicts major adverse cardiovascular events or all-cause death in patients with potentially curable lung cancer without a history of cardiovascular disease[J]. Heart Vessels, 2020, 35(11): 1483-1493. doi: 10.1007/s00380-020-01624-x [24] 蒋旭, 苗雷, 杨琳, 等. 小细胞肺癌影像诊断研究进展[J]. 中华全科医学, 2024, 22(2): 296-300. doi: 10.16766/j.cnki.issn.1674-4152.003388JIANG X, MIAO L, YANG L, et al. Advances in diagnostic imaging of small cell lung cancer[J]. Chinese Journal of General Practice, 2024, 22(2): 296-300. doi: 10.16766/j.cnki.issn.1674-4152.003388 -





 下载:
下载: