Predictive analysis of GBS colonization load on adverse pregnancy outcomes in patients with GBS infection in late pregnancy
-
摘要:
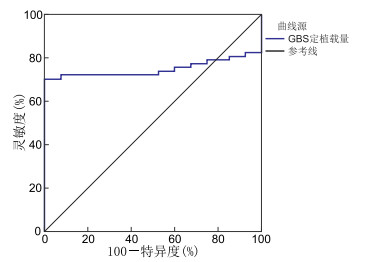
目的 分析B族链球菌(GBS)定植载量对妊娠晚期GBS感染患者不良妊娠结局的预测价值,并分析其作为预测指标的临床价值,为早期风险分层与干预提供依据。 方法 选取2022年1月—2024年12月绍兴市妇幼保健院收治的800例妊娠晚期GBS感染患者,随访至分娩,分析妊娠结局。根据妊娠结局,将患者分为不良妊娠结局组(247例)与良好妊娠结局组(553例),比较2组一般资料,使用logistic回归分析研究患者不良妊娠结局的影响因素,采用ROC曲线评估GBS定植载量对不良妊娠结局的预测价值。 结果 GBS感染组患者发生不良妊娠结局247例,发生率为30.88%。不良妊娠结局组与良好妊娠结局组的年龄、分娩孕周、多胎妊娠、肥胖、既往感染史、合并妊娠期糖尿病、合并妊娠期高血压、孕期用药、口腔卫生状况、GBS定植载量比较差异均有统计学意义(P<0.05)。Logistic回归分析显示,年龄大、分娩孕周小、多胎妊娠、肥胖、既往感染史、合并妊娠期糖尿病、合并妊娠期高血压、孕期用药、GBS定植载量高是影响患者不良妊娠结局的危险因素,口腔卫生状况良好是其保护因素。GBS定植载量对不良妊娠结局预测的AUC、灵敏度、特异度分别为0.828、69.39%、88.57%。 结论 GBS定植载量对妊娠晚期GBS感染患者不良妊娠结局具有较高的预测价值,临床可依据GBS定植载量水平,结合其他危险因素,对患者进行更精准的风险评估与个性化干预。 Abstract:Objective To analyze the predictive value of group B Streptococcus (GBS) colonization load for adverse pregnancy outcomes in patients with GBS infection in the third trimester of pregnancy, and to evaluate its clinical value as a predictive indicator for early risk stratification and intervention. Methods A total of 800 patients with GBS infection in the third trimester of pregnancy at Shaoxing Maternal and Child Health Hospital from January 2022 to December 2024 were selected, followed up until delivery, and their pregnancy outcomes of these patients were then analyzed. According to the pregnancy outcomes, the patients were divided into two groups: an adverse pregnancy outcome group and a good pregnancy outcome group, and the differences in general data between these two groups were then compared. Logistic regression was utilized in order to analyze the factors associated with adverse pregnancy outcomes in patients. The receiver operating characteristic (ROC) curve was utilized to evaluate the predictive value of GBS colonization load for adverse pregnancy outcomes. Results A total of 247 cases of adverse pregnancy outcomes were documented, with an incidence rate of 30.88%. Comparisons between the adverse pregnancy outcome group and the good pregnancy outcome group in terms of age, gestational age at delivery, multiple pregnancies, obesity, history of previous infections, complicated with gestational diabetes, complicated with gestational hypertension, medication during pregnancy, oral hygiene status, and GBS colonization load showed statistically significant differences (P < 0.05). Logistic regression analysis demonstrated that older age, smaller gestational age at delivery, multiple pregnancies, obesity, history of previous infections, complicated with gestational diabetes, complicated with gestational hypertension, medication during pregnancy, and high GBS colonization load were risk factors for adverse pregnancy outcomes in patients, while good oral hygiene status was a protective factor. The area under the curve (AUC), sensitivity, and specificity of GBS colonization load in predicting adverse pregnancy outcomes were 0.828, 69.39% and 88.57%, respectively. Conclusion It has been determined that the GBS colonization load possesses a high predictive value for adverse pregnancy outcomes in patients with GBS infection during the third trimester of pregnancy. Clinically, more accurate risk assessment and provide a personalized intervention for patients can be carried out based on the level of GBS colonization load combined with other risk factors. -
表 1 不良妊娠结局组与良好妊娠结局组患者一般资料比较
Table 1. Comparison of baseline characteristics between the adverse and favorable pregnancy outcome groups
项目 例数 不良妊娠结局组
(n=247)良好妊娠结局组
(n=553)统计量 P值 年龄(x±s,岁) 32.34±3.91 29.15±3.86 10.756a <0.001 分娩孕周(x±s,周) 36.25±1.10 38.52±1.24 24.747a <0.001 多胎妊娠[例(%)] 15.329b <0.001 是 60 32(53.33) 28(46.67) 否 740 215(29.05) 525(70.95) 肥胖[例(%)] 18.083b <0.001 是 150 68(45.33) 82(54.67) 否 650 179(27.54) 471(72.46) 生育史[例(%)] 0.041b 0.840 有 433 135(31.18) 298(68.82) 无 367 112(30.52) 255(69.48) 剖宫产史[例(%)] 0.301b 0.583 有 137 45(32.85) 92(67.15) 无 663 202(30.47) 461(69.53) 既往感染史[例(%)] 24.673b <0.001 有 192 87(45.31) 105(54.69) 无 608 160(26.32) 448(73.68) 合并妊娠期糖尿病[例(%)] 8.987b 0.003 是 134 56(41.79) 78(58.21) 否 666 191(28.68) 475(71.32) 合并妊娠期高血压[例(%)] 10.457b 0.001 是 95 43(45.26) 52(54.74) 否 705 204(28.94) 501(71.06) 孕期用药[例(%)] 14.991b <0.001 有 178 76(42.70) 102(57.30) 无 622 171(27.49) 451(72.51) 口腔卫生状况[例(%)] 24.186b <0.001 良好 487 119(24.44) 368(75.56) 不良 313 128(40.89) 185(59.11) 孕期运动[例(%)] 0.145b 0.704 有规律 283 85(30.04) 198(69.96) 无规律 517 162(31.33) 355(68.67) 居住环境[例(%)] 0.149b 0.699 良好 670 205(30.60) 465(69.40) 不良 130 42(32.31) 88(67.69) GBS定植载量[例(%)] 58.463b <0.001 高载量 345 156(45.22) 189(54.78) 低载量 455 91(20.00) 364(80.00) 注:a为t值,b为χ2值。 表 2 变量赋值情况
Table 2. Variable assignment
变量 赋值方法 年龄 连续变量,以实际值赋值 分娩孕周 连续变量,以实际值赋值 多胎妊娠 是=1,否=0 肥胖 是=1,否=0 既往感染史 有=1,无=0 合并妊娠期糖尿病 是=1,否=0 合并妊娠期高血压 是=1,否=0 孕期用药 有=1,无=0 口腔卫生状况 良好=1,不良=0 GBS定植载量 高载量=1,低载量=0 表 3 影响患者不良妊娠结局的多因素logistic回归分析
Table 3. Multivariate Logistic analysis of factors influencing adverse pregnancy outcomes in patients
变量 B SE Waldχ2 P值 OR(95% CI) 年龄 0.570 0.152 21.933 <0.001 1.752(1.238~2.924) 分娩孕周 0.469 0.206 15.882 <0.001 2.095(1.525~6.881) 多胎妊娠 1.233 0.298 20.053 <0.001 3.152(2.161~5.827) 肥胖 0.962 0.216 27.342 <0.001 2.714(1.657~3.841) 既往感染史 1.122 0.254 23.946 <0.001 3.751(1.874~4.507) 合并妊娠期糖尿病 0.771 0.196 22.775 <0.001 2.102(1.591~3.352) 合并妊娠期高血压 0.844 0.183 20.306 <0.001 2.304(1.517~3.963) 孕期用药 0.951 0.266 16.406 <0.001 2.342(1.743~3.799) 口腔卫生状况 -0.154 0.557 6.588 0.027 0.880(0.726~0.961) GBS定植载量 1.344 0.272 23.652 <0.001 3.720(2.268~6.427) -
[1] 施锦金, 蔡锋成, 张晶, 等. 妊娠晚期生殖道B族链球菌感染危险因素及其妊娠结局[J]. 中华医院感染学杂志, 2024, 34(9): 1405-1408.SHI J J, CAI F C, ZHANG J, et al. Risk factors of genital tract group B streptococcal infection in late pregnancy and its pregnancy outcomes[J]. Chinese Journal of Nosocomiology, 2024, 34(9): 1405-1408. [2] YANNI M, STARK M, FRANCIS L, et al. Neonatal group B streptococcal infection in Australia: a case-control study[J]. Pediatr Infect Dis J, 2023, 42(5): 429-435. doi: 10.1097/INF.0000000000003881 [3] 王婷婷, 薛飞扬, 綦萍, 等. 妊娠晚期孕妇生殖道B族链球菌感染对并发胎膜早破与新生儿感染、围生结局影响[J]. 中国计划生育学杂志, 2022, 30(6): 1348-1351.WANG T T, XUE F Y, QI P, et al. Impact of genital tract group B streptococcal infection in late-pregnancy women on concurrent premature rupture of membranes, neonatal infection and perinatal outcomes[J]. Chinese Journal of Family Planning, 2022, 30(6): 1348-1351. [4] 黄金瑞, 梁海峰, 黄玲玲. B族链球菌感染对高危妊娠孕晚期孕妇母婴结局影响[J]. 中国计划生育学杂志, 2023, 31(6): 1474-1477.HUANG J R, LIANG H F, HUANG L L. Influence of group B streptococcal infection on maternal and infant outcomes in high-risk pregnant women in late pregnancy[J]. Chinese Journal of Family Planning, 2023, 31(6): 1474-1477. [5] 杨晓杰, 宋俊霞, 张丽丽. 焦作地区妊娠晚期生殖道B族溶血性链球菌感染流行情况及对妊娠结局的影响[J]. 医药论坛杂志, 2024, 45(8): 864-868.YANG X J, SONG J X, ZHANG L L. Prevalence of genital tract group B streptococcal infection in late pregnancy in Jiaozuo area and its impact on pregnancy outcomes[J]. Journal of Medical Forum, 2024, 45(8): 864-868. [6] MA H, XU J W, ZHANG Y H, et al. The current status of group B streptococcus infection in the reproductive tract of late-pregnancy women and its impact on pregnancy outcomes[J]. Arch Gynecol Obstet, 2024, 310(2): 1151-1155. doi: 10.1007/s00404-023-07343-8 [7] 金彩凤, 吴玮, 吴轲. B族链球菌感染及阴道微生态变化与不良妊娠结局的关系[J]. 天津医药, 2024, 52(8): 858-862.JIN C F, WU W, WU K. Relationship between group B streptococcal infection, changes in vaginal microecology and adverse pregnancy outcomes[J]. Tianjin Medical Journal, 2024, 52(8): 858-862. [8] 丁小梅, 张亿林. 孕晚期B族链球菌感染差异及其对妊娠结局和新生儿的影响[J]. 热带医学杂志, 2024, 24(2): 251-254.DING X M, ZHANG Y L. Differences in group B streptococcal infection in late pregnancy and its impact on pregnancy outcomes and newborns[J]. Journal of Tropical Medicine, 2024, 24(2): 251-254. [9] 茆政, 应斐, 崔凡. 孕妇B族链球菌带菌妊娠与不良妊娠结局的关系[J]. 安徽医学, 2021, 42(4): 397-399.MAO Z, YING F, CUI F. Association between maternal group B streptococcus carrier pregnancy and adverse pregnancy outcomes[J]. Anhui Medical Journal, 2021, 42(4): 397-399. [10] 敖凤, 范玉兰, 李佳黛, 等. 孕晚期孕妇B族链球菌感染的分布特征、危险因素分析及对生殖道微生物和妊娠结局的影响[J]. 现代生物医学进展, 2024, 24(13): 2516-2520.AO F, FAN Y L, LI J D, et al. Distribution characteristics, risk factor analysis of group B streptococcal infection in late-pregnancy women and its impact on genital tract microorganisms and pregnancy outcomes[J]. Progress in Modern Biomedicine, 2024, 24(13): 2516-2520. [11] 杨艳丽, 赵维英. 妊娠晚期发生B族链球菌感染的危险因素及血清CCL-1水平的预测价值分析[J]. 热带医学杂志, 2023, 23(12): 1715-1718, 1741.YANG Y L, ZHAO W Y. Risk factors of group B streptococcal infection in late pregnancy and predictive value of serum CCL-1 level[J]. Journal of Tropical Medicine, 2023, 23(12): 1715-1718, 1741. [12] 许云, 姚金翠, 孔木飞, 等. 孕晚期孕妇B族链球菌感染情况及不良妊娠结局分析[J]. 中国病原生物学杂志, 2024, 19(4): 463-467.XU Y, YAO J C, KONG M F, et al. Status of group B streptococcal infection in late-pregnancy women and analysis of adverse pregnancy outcomes[J]. Journal of Pathogen Biology, 2024, 19(4): 463-467. [13] PAUL P, GONCALVES B P, LE DOARE K, et al. 20 million pregnant women with group B streptococcus carriage: consequences, challenges, and opportunities for prevention[J]. Curr Opin Pediatr, 2023, 35(2): 223-230. doi: 10.1097/MOP.0000000000001223 [14] 吴娟, 晏敏, 万红芳, 等. 血清25-羟基维生素D3水平对妊娠晚期B族链球菌感染孕妇发生胎膜早破的影响[J]. 热带医学杂志, 2023, 23(10): 1413-1417.WU J, YAN M, WAN H F, et al. Influence of serum 25-hydroxyvitamin D3 level on premature rupture of membranes in late-pregnancy women with group B streptococcal infection[J]. Journal of Tropical Medicine, 2023, 23(10): 1413-1417. [15] 程贤鹦, 王园园, 张朋辉, 等. 三孩政策后孕产妇妊娠特征, 分娩方式和围生儿结局的临床研究[J]. 中华全科医学, 2024, 22(3): 451-454, 477. doi: 10.16766/j.cnki.issn.1674-4152.003424CHENG X Y, WANG Y Y, ZHANG P H, et al. Clinical study on pregnancy characteristics, delivery modes and perinatal outcomes of pregnant women after the three-child policy[J]. Chinese Journal of General Practice, 2024, 22(3): 451-454, 477. doi: 10.16766/j.cnki.issn.1674-4152.003424 [16] 陈佳佳, 王文强. 孕晚期无症状B族链球菌感染对阴道微生态环境及母儿结局的影响[J]. 中华医院感染学杂志, 2024, 34(14): 2211-2215.CHEN J J, WANG W Q. Impact of asymptomatic group B streptococcal infection in late pregnancy on vaginal microecological environment and maternal and infant outcomes[J]. Chinese Journal of Nosocomiology, 2024, 34(14): 2211-2215. [17] KARAMPATSAS K, DAVIES H, MYNAREK M, et al. Clinical risk factors associated with late-onset invasive group B streptococcal disease: systematic review and meta-analyses[J]. Clin Infect Dis, 2022, 75(7): 1255-1264. doi: 10.1093/cid/ciac206 [18] 樊红娟, 倪明, 吴静, 等. 孕晚期生殖道定植B族链球菌对妊娠结局的影响及其耐药性与耐药基因[J]. 中华医院感染学杂志, 2023, 33(24): 3776-3779.FAN H J, NI M, WU J, et al. Impact of genital tract colonization of group B streptococcus in late pregnancy on pregnancy outcomes and its drug resistance and resistance genes[J]. Chinese Journal of Nosocomiology, 2023, 33(24): 3776-3779. [19] 张科伟, 杨菲菲, 徐静, 等. 孕晚期血清sTREM-1、HBD2水平与B族链球菌感染顺产孕妇新生儿结局关系分析[J]. 中国病原生物学杂志, 2024, 19(6): 703-706, 714.ZHANG K W, YANG F F, XU J, et al. Analysis of relationship between serum sTREM-1 and HBD2 levels in late pregnancy and neonatal outcomes of parturient women with group B streptococcal infection delivered vaginally[J]. Journal of Pathogen Biology, 2024, 19(6): 703-706, 714. [20] 马亚军, 晁利娜, 陈玉明. 新乡地区妊娠晚期孕妇生殖道GBS感染情况及其对胎膜早破和妊娠结局的影响[J]. 热带医学杂志, 2023, 23(2): 203-207.MA Y J, CHAO L N, CHEN Y M. Status of genital tract GBS infection in late-pregnancy women in Xinxiang area and its impact on premature rupture of membranes and pregnancy outcomes[J]. Journal of Tropical Medicine, 2023, 23(2): 203-207. [21] 林建丽, 凌奕, 陈华, 等. B族链球菌感染对孕妇阴道微生态失衡和血清炎性因子与母婴结局的影响[J]. 中华医院感染学杂志, 2022, 32(3): 462-465.LIN J L, LING Y, CHEN H, et al. Impact of group B streptococcal infection on vaginal microecological imbalance, serum inflammatory factors and maternal and infant outcomes in pregnant women[J]. Chinese Journal of Nosocomiology, 2022, 32(3): 462-465. [22] 胡毅娜, 周定杰, 吴玉璘, 等. 孕晚期孕妇生殖道GBS感染及预防性治疗与妊娠结局和新生儿预后的关系[J]. 中国优生与遗传杂志, 2023, 31(12): 2472-2477.HU Y N, ZHOU D J, WU Y L, et al. Relationship between genital tract GBS infection in late-pregnancy women, preventive treatment and pregnancy outcomes and neonatal prognosis[J]. Chinese Journal of Birth Health & Heredity, 2023, 31(12): 2472-2477. -





 下载:
下载: