Establishment of a nomogram prediction model for the risk of hypoxic-ischemic encephalopathy in neonates with intrauterine distress
-
摘要:
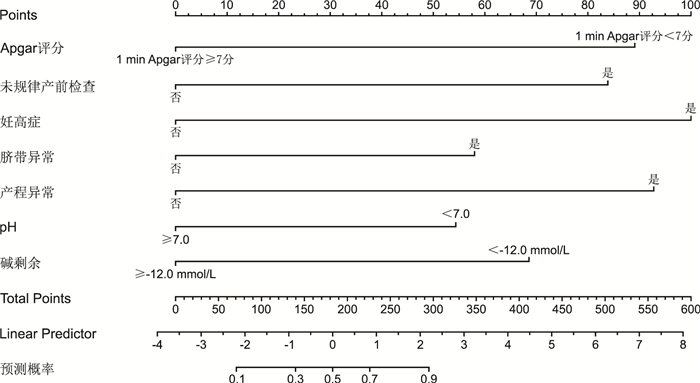
目的 分析宫内窘迫新生儿发生缺氧缺血性脑病(HIE)的危险因素,并构建个体化列线图预测模型。 方法 收集2017年1月—2021年12月淮安市第二人民医院新生儿科收治的具有宫内窘迫暴露因素且发生HIE的新生儿96例(病例组),另选择同期本院收治的具有宫内窘迫暴露因素但未发生HIE的新生儿96例(对照组),采用logistic回归分析筛选影响宫内窘迫新生儿发生HIE的危险因素;采用R软件构建列线图模型,同时进行模型验证。 结果 1 min Apgar评分<7分(P < 0.001)、不规律产前检查(P=0.003)、妊高症(P < 0.001)、脐带异常(P=0.043)、产程异常(P=0.001)、pH < 7.0(P=0.009)、碱剩余 < -12.0 mmol/L(P=0.003)是宫内窘迫新生儿发生HIE的独立危险因素。ROC曲线下面积为0.875(95% CI:0.826~0.925)。校准曲线斜率接近1,且H-L拟合优度检验χ2=7.221,P=0.513。 结论 1 min Apgar评分<7分、不规律产前检查、妊高症、脐带异常、产程异常、pH < 7.0、碱剩余 < -12.0 mmol/L均是宫内窘迫新生儿发生HIE的独立危险因素,根据以上指标构建的列线图预测模型具有较好的预测效能,能准确预测宫内窘迫新生儿发生HIE风险。 Abstract:Objective To analyze the risk factors for hypoxic-ischemic encephalopathy (HIE) in neonates with intrauterine distress, and to develop a personalized nomograph prediction model. Methods Ninety-six neonates with exposure factors of intrauterine distress and HIE (case group) treated in the Neonatology Department of Huaian Second People ' s Hospital from January 2017 to December 2021 were collected, 96 neonates with exposure factors of intrauterine distress who did not develop HIE (control group) treated in our hospital during the same period were selected. Logistic regression analysis was performed to screen the risk factors affecting the risk of HIE in neonates with intrauterine distress; R software was used to construct a nomogram model to predict the risk of HIE in neonates with intrauterine distress, and the model was meanwhile validated. Results 1 min Apgar score < 7 points (P < 0.001), irregular prenatal examination (P=0.003), pregnancy-induced hypertension (P < 0.001), abnormal umbilical cord (P=0.043), abnormal labor process (P=0.001), pH < 7.0 (P=0.009), alkaline residue < -12.0 mmol/L (P=0.003) were independent risk factors for HIE in neonates with intrauterine distress. The area under the ROC curve was 0.875 (95% CI: 0.826-0.925). The slope of the calibration curve was close to 1, and the H-L goodness-of-fit test χ2=7.221, P=0.513. Conclusion 1 min Apgar score < 7, irregular prenatal examination, pregnancy induced hypertension, umbilical cord abnormality, abnormal labor process, pH < 7.0, and alkaline residue < -12.0 mmol/L are all independent risk factors for HIE in neonates with intrauterine distress. The nomograph prediction model constructed using the above indicators has good predictive power and can accurately predict the risk of HIE in neonates with intrauterine distress. -
表 1 宫内窘迫新生儿发生HIE风险的单因素分析
Table 1. Univariate analysis of the risk of HIE in neonates with intrauterine distress
项目 病例组(96例) 对照组(96例) 统计量 P值 新生儿性别[例(%)] 男 75(78.13) 53(55.21) 11.344a 0.001 女 21(21.88) 43(44.79) 胎龄(x±s,周) 40.93±1.82 40.48±2.07 1.600b 0.111 新生儿类别[例(%)] 足月新生儿 70(72.92) 92(95.83) 19.121a < 0.001 过期产儿 26(27.08) 4(4.17) 新生儿出生时体质量(x±s,g) 2 864.78±402.94 3 146.47±542.36 4.085b < 0.001 小于胎龄儿[例(%)] 12(12.50) 9(9.38) 0.481a 0.488 大于胎龄儿[例(%)] 2(2.08) 3(3.13) 0.205a 0.650 Apgar评分(1 min)<7分[例(%)] 是 51(53.13) 20(20.83) 21.477a < 0.001 否 45(46.88) 76(79.17) Apgar评分(5 min)<7分[例(%)] 是 24(25.00) 8(8.33) 9.600a 0.002 否 72(75.00) 88(91.67) 新生儿呼吸性酸中毒[例(%)] 是 45(46.88) 17(17.71) 18.676a < 0.001 否 51(53.13) 79(82.29) 孕妇年龄(x±s,岁) 29.63±5.24 28.82±4.93 1.103b 0.271 母亲职业[例(%)] 知识分子 14(14.58) 20(20.83) 6.160a 0.104 工人 12(12.50) 21(21.88) 农民 20(20.83) 20(20.83) 无业 50(52.08) 35(36.46) 父亲职业[例(%)] 知识分子 18(18.75) 25(26.04) 16.157a 0.001 工人 23(23.96) 37(38.54) 农民 18(18.75) 21(21.88) 无业 37(38.54) 13(13.54) 高龄产妇[例(%)] 是 31(32.29) 17(17.71) 5.444a 0.020 否 65(67.71) 79(82.29) 首次妊娠[例(%)] 是 53(55.21) 72(75.00) 8.276a 0.004 否 43(44.79) 24(25.00) 不规律产前检查[例(%)] 是 29(30.21) 9(9.38) 13.124a < 0.001 否 67(69.79) 87(90.63) 妊娠期贫血[例(%)] 是 27(28.13) 10(10.42) 9.675a 0.002 否 69(71.88) 86(89.58) 妊高症[例(%)] 是 36(37.50) 11(11.46) 17.608a < 0.001 否 60(62.50) 85(88.54) GDM[例(%)] 是 29(30.21) 14(14.58) 6.743a 0.009 否 67(69.79) 82(85.42) 羊水污染[例(%)] 是 31(32.29) 3(3.13) 28.021a < 0.001 否 65(67.71) 93(96.88) 羊水过少[例(%)] 是 12(12.50) 6(6.25) 2.207a 0.137 否 84(87.50) 90(93.75) 脐带异常[例(%)] 是 33(34.38) 8(8.33) 19.383a < 0.001 否 63(65.63) 88(91.67) 胎盘早剥[例(%)] 是 12(12.50) 2(2.08) 7.705a 0.006 否 84(87.50) 94(97.92) 前置胎盘[例(%)] 是 14(14.58) 11(11.46) 0.414a 0.520 否 82(85.42) 85(88.54) 产程异常[例(%)] 是 35(36.46) 10(10.42) 18.141a < 0.001 否 61(63.54) 86(89.58) 分娩方式[例(%)] 自然分娩 59(61.46) 55(57.29) 0.345a 0.557 剖宫产 37(38.54) 41(42.71) pH[例(%)] < 7.0 75(78.13) 50(52.08) 14.328a < 0.001 ≥7.0 21(21.88) 46(47.92) 碱剩余[例(%)] <-12.0 mmol/L 83(86.46) 56(58.33) 18.999a < 0.001 ≥-12.0 mmol/L 13(13.54) 40(41.67) 二氧化碳分压(x±s,mmHg) 80.35±10.06 70.46±9.75 6.917b < 0.001 氧分压(x±s,mmHg) 14.48±2.02 16.02±2.29 4.941b < 0.001 碳酸氢根(x±s,mmol/L) 18.62±2.39 20.75±2.46 6.085b < 0.001 注:a为χ2值,b为t值;1 mmHg=0.133 kPa。 表 2 变量赋值情况
Table 2. Variable assignment
变量 类别 赋值方法 因变量 宫内窘迫新生儿是否发生HIE 否=0,是=1 自变量 新生儿性别 女=0,男=1 新生儿 足月新生儿=0,过期产儿=1 新生儿出生时体质量 以实际值赋值 Apgar评分(1 min)<7分 否=0,是=1 Apgar评分(5 min)<7分 否=0,是=1 新生儿呼吸性酸中毒 否=0,是=1 父亲职业 知识分子=(0, 0, 0),工人=(1, 0, 0),农民=(0, 1, 0),无业=(0, 0, 1),以知识分子为参照 高龄产妇 否=0,是=1 首次妊娠 是=0,否=1 不规律产前检查 否=0,是=1 妊娠期贫血 否=0,是=1 妊高症 否=0,是=1 GDM 否=0,是=1 羊水污染 否=0,是=1 脐带异常 否=0,是=1 胎盘早剥 否=0,是=1 产程异常 否=0,是=1 pH ≥7.0=0, < 7.0=1 碱剩余 ≥-12.0 mmol/L=0, < -12.0 mmol/L=1 二氧化碳分压 以实际值赋值 氧分压 以实际值赋值 碳酸氢根 以实际值赋值 表 3 宫内窘迫新生儿发生HIE风险的多因素logistic回归分析
Table 3. Multivariate logistic regression analysis of the risk of HIE in neonates with intrauterine distress
因素 B SE Waldχ2 P值 OR值 95% CI Apgar评分 1.747 0.431 16.468 0.000 5.738 2.468~13.341 未规律产前检查 1.644 0.555 8.777 0.003 5.178 1.745~15.368 妊高症 1.961 0.484 16.386 0.000 7.104 2.749~18.356 脐带异常 1.137 0.563 4.082 0.043 3.118 1.035~9.399 产程异常 1.819 0.553 10.819 0.001 6.167 2.086~18.233 pH 1.066 0.408 6.834 0.009 2.904 1.306~6.458 碱剩余 1.344 0.452 8.860 0.003 3.836 1.583~9.297 -
[1] 陈莉, 陈信. 持续脑功能监测在新生儿缺氧缺血性脑病的应用效果[J]. 中华全科医学, 2020, 18(4): 564-567. doi: 10.16766/j.cnki.issn.1674-4152.001299CHEN L, CHEN X. Effect of continuous brain function monitoring on neonatal hypoxic-ischemic encephalopathy[J]. Chinese Journal of General Practice, 2020, 18(4): 564-567. doi: 10.16766/j.cnki.issn.1674-4152.001299 [2] GRECO P, NENCINI G, PIVA I, et al. Pathophysiology of hypoxic-ischemic encephalopathy: a review of the past and a view on the future[J]. Acta Neurol Belg, 2020, 120(2): 277-288. doi: 10.1007/s13760-020-01308-3 [3] 刘珍, 赵延凤, 魏莹亚, 等. 新生儿发生缺氧缺血性脑病的影响因素分析[J]. 临床医学研究与实践, 2020, 5(30): 1-2, 6. https://www.cnki.com.cn/Article/CJFDTOTAL-YLYS202030002.htmLIU Z, ZHAO Y F, WEI Y Y, et al. Analysis of influencing factors of neonatal hypoxic ischemic encephalopathy[J]. Clinical Research and Practice, 2020, 5(30): 1-2, 6. https://www.cnki.com.cn/Article/CJFDTOTAL-YLYS202030002.htm [4] 于扬, 司振妍, 吕聪聪. 3.0T核磁共振磁敏感加权成像在新生儿缺氧缺血性脑病诊断中的价值分析[J]. 中国基层医药, 2019, 26(3): 272-275. doi: 10.3760/cma.j.issn.1008-6706.2019.03.005YU Y, SI Z Y, LYU C C. Clinical value of 3.0T magnetic resonance magnetic sensitive weighted imaging in the diagnosis of neonatal hypoxic ischemic encephalopathy[J]. Chinese Journal of Primary Medicine and Pharmacy, 2019, 26(3): 272-275. doi: 10.3760/cma.j.issn.1008-6706.2019.03.005 [5] 付仕强, 邓小梅, 张程. 头针联合康复训练对缺氧缺血性脑病患儿近期预后的影响[J]. 海南医学, 2017, 28(14): 2375-2377. doi: 10.3969/j.issn.1003-6350.2017.14.046FU S Q, DENG X M, ZHANG C. Influence of scalp acupuncture combined with rehabilitation training on the short-term prognosis of children with hypoxic ischemic encephalopathy[J]. Hainan Medical Journal, 2017, 28(14): 2375-2377. doi: 10.3969/j.issn.1003-6350.2017.14.046 [6] YASUDA S, SUZUKI H, HTUN Y, et al. Hour-specific nomogram for transcutaneous Bilirubin in newborns in Myanmar[J]. Pediatr Int, 2020, 62(9): 1049-1053. doi: 10.1111/ped.14251 [7] HESS D R. A nomogram for use of non-invasive respiratory strategies in COVID-19[J]. Lancet Digit Health, 2021, 3(3): e140-e141. doi: 10.1016/S2589-7500(21)00006-6 [8] 谢幸, 苟文丽. 妇产科学[M]. 8版. 北京: 人民卫生出版社, 2013: 118-120.XIE X, GOU W L. Gynecology and Obstetrics[M]. 8th Ed. Beijing: People's Medical Publishing House, 2013: 118-120. [9] 果崇慧, 杨青. 神经节苷脂治疗新生儿缺氧缺血性脑病对患儿血清炎症相关细胞因子和MMP-9的影响[J]. 河北医药, 2018, 40(2): 219-223. https://www.cnki.com.cn/Article/CJFDTOTAL-HBYZ201802014.htmGUO Z H, YANG Q. Effects of ganglioside on serum inflammatory cytokines and MMP-9 in neonates with hypoxic-ischemic encephalopathy[J]. Hebei Medical Journal, 2018, 40(2): 219-223. S https://www.cnki.com.cn/Article/CJFDTOTAL-HBYZ201802014.htm [10] WASSINK G, DAVIDSON J O, DHILLON S K, et al. Therapeutic hypothermia in neonatal hypoxic-ischemic encephalopathy[J]. Curr Neurol Neurosci Rep, 2019, 19(2): 2. [11] CNATTINGIUS S, JOHANSSON S, RAZAZ N. Apgar score and risk of neonatal death among preterm infants[J]. N Engl J Med, 2020, 383(1): 49-57. doi: 10.1056/NEJMoa1915075 [12] 赵燕凤, 张志群, 芦蕙, 等. 脐动脉血气分析联合Apgar评分对新生儿窒息多器官损害的诊断意义[J]. 中华全科医学, 2017, 15(2): 267-269. doi: 10.16766/j.cnki.issn.1674-4152.2017.02.026ZHAO Y F, ZHANG Z Q, LU H, et al. Umbilical artery blood gas analysis and Apgar score for multiple organ damage after neonatal asphyxia[J]. Chinese Journal of General Practice, 2017, 15(2): 267-269. doi: 10.16766/j.cnki.issn.1674-4152.2017.02.026 [13] BUTT T K, FAROOQUI R, KHAN M A. Risk factors for hypoxic ischemic encephalopathy in children[J]. J Coll Physicians Surg Pak, 2008, 18(7): 428-432. [14] 曹芳, 江余明, 肖佳荔, 等. 新生儿缺氧缺血性脑病的影响因素及不同亚低温时间窗治疗效果分析[J]. 中国基层医药, 2022, 29(9): 1369-1374.CAO F, JIANG Y M, XIAO J L, et al. Influential factors of neonatal hypoxic ischemic encephalopathy and the therapeutic effects of mild hypothermia at different time windows[J]. Chinese Journal of Primary Medicine and Pharmacy, 2022, 29(9): 1369-1374. [15] 尹崇兰. 新生儿缺血缺氧性脑病发生的相关危险因素研究[J]. 中国妇幼健康研究, 2017, 28(6): 630-631, 635. https://www.cnki.com.cn/Article/CJFDTOTAL-SANE201706004.htmYIN C L. Risk factors of neonatal hypoxic ischemia encephalopathy[J]. Chinese Journal of Woman and Child Health Research, 2017, 28(6): 630-631, 635. https://www.cnki.com.cn/Article/CJFDTOTAL-SANE201706004.htm [16] NASIELL J, PAPADOGIANNAKIS N, LÖF E, et al. Hypoxic ischemic encephalopathy in newborns linked to placental and umbilical cord abnormalities[J]. J Matern Fetal Neonatal Med, 2016, 29(5): 721-726. [17] TORBENSON V E, TOLCHER M C, NESBITT K M, et al. Intrapartum factors associated with neonatal hypoxic ischemic encephalopathy: a case-controlled study[J]. BMC Pregnancy Childbirth, 2017, 17(1): 415. [18] FERREIRA C S, MELO Â, FACHADA A H, et al. Umbilical cord blood gas analysis, obstetric performance and perinatal outcome[J]. Rev Bras Ginecol Obstet, 2018, 40(12): 740-748. [19] LILJESTROM L, WIKSTROM A K, AGREN J, et al. Antepartum risk factors for moderate to severe neonatal hypoxic ischemic encephalopathy: a Swedish national cohort study[J]. Acta Obstet Gynecol Scand, 2018, 97(5): 615-623. [20] PEEBLES P J, DUELLO T M, EICKHOFF J C, et al. Antenatal and intrapartum risk factors for neonatal hypoxic ischemic encephalopathy[J]. J Perinatol, 2020, 40(1): 63-69. -





 下载:
下载: