Correlation between preoperative serum osmotic pressure level and hospitalization time and complication risk of elderly patients with femoral neck fracture
-
摘要:
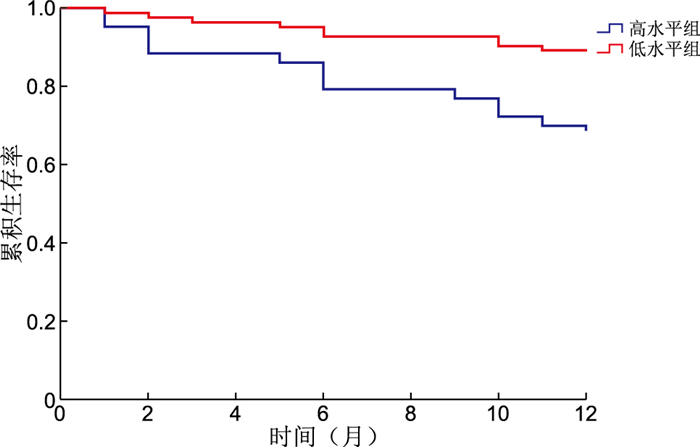
目的 分析老年股骨颈骨折患者的术前血清渗透压水平,并探讨其水平高低与住院时间以及并发症发生风险的关系。 方法 选取2020年1月—2021年12月于浙江中医药大学附属温州中西医结合医院接受治疗的120例股骨颈骨折患者作为研究对象,根据患者术前的血清渗透压水平将患者分为高水平组和低水平组,收集患者相关临床资料,同时进行为期1年的随访,记录患者全因死亡情况。采用Spearman相关性分析研究术前血清渗透压水平与患者住院时间、并发症等的相关性,采用Cox回归分析研究老年股骨颈骨折患者存活率的影响因素。 结果 41例患者纳入高水平组,79例患者纳入低水平组。术前血清渗透压水平与多维预后指数(MPI)得分(r=0.501)、住院时间(r=0.496)、术后并发症(r=0.383)的发生均呈正相关关系(P<0.05);Cox回归分析显示,性别(HR=17.404)、血清渗透压水平(HR=1.136)、MPI(HR=1.294)、格拉斯哥预后评分(GPS,HR=0.114)均是老年股骨颈骨折患者术后死亡的影响因素,在校正性别、MPI评分、GPS评分后的Cox回归分析中发现,术前血清渗透压水平(HR=1.071)是老年股骨颈骨折患者术后死亡的独立影响因素(P<0.05)。 结论 老年股骨颈骨折患者的住院时间、并发症发生情况与术前的血清渗透压水平和虚弱程度有关,术前进行血清渗透压水平检查,有助于围手术期进行更充分的液体管理,以降低术后的死亡风险。 Abstract:Objective To analyze the preoperative serum osmotic pressure level of elderly patients with femoral neck fracture, and to explore the relationship between its level and hospitalization time and the risk of complications. Methods A total of 120 patients with femoral neck fracture who were treated in Wenzhou Hospital of Integrated Traditional Chinese and Western Medicine Affiliated to Zhejiang University of Traditional Chinese Medicine from January 2020 to December 2021 were selected as the research object. According to the preoperative serum osmotic pressure level of patients, patients were divided into high-level group and low-level group. The clinical data of patients were collected and followed up for one year to record all-cause deaths. Spearman correlation was used to analyze the correlation between preoperative serum osmotic pressure level and hospitalization time and complications, and Cox regression was used to analyze the influencing factors of survival rate of elderly patients with femoral neck fracture. Results Forty-one patients were included in the high-level group and 79 in the low-level group. Preoperative serum osmotic pressure level was positively correlated with MPI score (r=0.501), hospital stay (r=0.496) and postoperative complications (r=0.383), P<0.05. Cox regression analysis showed that gender (HR=17.404), serum osmolality level (HR=1.136), MPI score (HR=1.294) and GPS score (HR=0.114) were all influencing factors for postoperative death in elderly patients with femoral neck. Cox regression analysis after adjusting for gender, MPI score and GPS score found that preoperative serum osmolality level (HR=1.071) was an independent determinant of postoperative death in elderly femoral neck patients (P<0.05). Conclusion The hospitalization time and complications of elderly patients with femoral neck fracture are related to the preoperative serum osmotic pressure level and the degree of weakness. Preoperative examination of serum osmotic pressure level is helpful for more adequate perioperative fluid management to reduce the risk of postoperative death. -
表 1 2组老年股骨颈骨折患者临床资料比较
Table 1. Comparison of clinical data in two groups of elderly patients with femoral neck fractures
项目 低水平组(n=79) 高水平组(n=41) 统计量 P值 年龄(x±s,岁) 77.16±5.34 79.26±4.69 2.217a 0.029 性别[例(%)] 0.216b 0.642 男性 20(25.31) 12(29.27) 女性 59(74.68) 29(70.73) BMI(x±s) 22.34±2.18 24.28±3.72 3.076a 0.003 合并症[例(%)] 高血压 41(51.90) 30(73.17) 5.055b 0.025 糖尿病 14(17.72) 12(29.27) 2.120b 0.145 冠心病 13(16.46) 8(19.51) 0.175b 0.676 慢性心衰 9(11.39) 9(21.95) 2.360b 0.124 慢性肾脏病 7(8.86) 10(24.39) 5.353b 0.021 COPD 9(11.39) 4(9.76) 0.075b 0.784 Na+(x±s,mmol/L) 137.25±3.26 141.30±4.22 5.370a <0.001 K+(x±s,mmol/L) 4.05±0.28 4.19±0.31 2.424a 0.018 空腹血糖(x±s,mmol/L) 6.94±1.11 7.86±1.88 2.883a 0.006 尿素(x±s,mmol/L) 6.75±1.79 11.09±2.08 11.355a <0.001 血清渗透压(x±s,mmol/L) 289.47±8.89 308.58±7.33 12.571a <0.001 血红蛋白(x±s,g/dL) 12.18±1.49 11.56±1.62 2.043a 0.045 CRP(x±s,mg/L) 29.45±4.49 30.49±5.62 1.027a 0.308 淋巴细胞(x±s,×103/mL) 1.06±0.11 1.10±0.13 1.682a 0.097 GPS(x±s,分) 6.11±0.87 5.89±0.71 1.487a 0.140 MPI(x±s,分) 0.81±0.04 0.87±0.05 6.657a <0.001 住院时间(x±s,d) 8.16±1.53 11.05±2.14 7.687a <0.001 术后并发症发生情况[例(%)] 急性呼吸衰竭 3(3.80) 5(12.20) 1.858b 1.173 肺炎 2(2.53) 3(7.32) 0.581b 0.446 谵妄 14(17.72) 12(29.27) 2.120b 0.145 电解质紊乱 12(15.19) 13(31.71) 4.465b 0.035 心律失常 5(6.33) 8(19.51) 4.856b 0.028 尿路感染 3(3.80) 2(4.88) 0.040b 0.841 压疮 1(1.27) 3(7.32) 1.477b 0.224 总发生[例(%)] 38(48.10) 30(73.17) 6.908b 0.009 注:a为t值,b为χ2值。部分患者发生2种或以上并发症。 表 2 术前血清渗透压与其他指标的相关性
Table 2. Correlation between preoperative serum osmolality and other indicators
项目 血清渗透压 MPI r值 P值 r值 P值 MPI 0.501 <0.001 住院时间 0.496 <0.001 0.436 <0.001 术后并发症 0.383 <0.001 0.341 <0.001 表 3 变量赋值方法
Table 3. Variable assignment methods
变量 赋值方法 是否死亡 是=1,否=0 性别 男性=1,女性=0 血清渗透压 连续变量,以实际值赋值 MPI 连续变量,以实际值赋值 GPS 连续变量,以实际值赋值 校正后血清渗透压 连续变量,以实际值赋值 表 4 影响股骨颈骨折患者术后死亡的Cox回归分析
Table 4. Cox Regression analysis of postoperative mortality in patients with femoral neck fractures
变量 B SE Waldχ2 P值 HR值 95% CI 性别 2.857 0.506 31.927 <0.001 17.404 6.461~46.880 血清渗透压 0.128 0.019 46.805 <0.001 1.136 1.095~1.178 MPI 0.257 0.034 56.960 <0.001 1.294 1.210~1.383 GPS -2.171 0.316 47.362 <0.001 0.114 0.061~0.212 校正后血清渗透压 0.069 0.030 5.072 0.024 1.071 1.009~1.137 -
[1] 刘蓬然, 张亚鑫, 孙斌磊, 等. 老年股骨颈骨折的危险因素[J]. 中南大学学报(医学版), 2021, 46(3): 272-277. https://www.cnki.com.cn/Article/CJFDTOTAL-HNYD202103009.htmLIU P R, ZHANG Y X, SUN B L, et al. Risk factors for femoral neck fracture in elderly population[J]. Journal of Central South University: Medical Science, 2021, 46(3): 272-277. https://www.cnki.com.cn/Article/CJFDTOTAL-HNYD202103009.htm [2] 赵锋, 颜峰, 孟利锋, 等. 股骨颈骨折患者术后爆发痛发生现状及影响因素分析[J]. 中华全科医学, 2022, 20(9): 1498-1501. doi: 10.16766/j.cnki.issn.1674-4152.002633ZHAO F, YAN F, MENG L F, et al. Current situation and influencing factors of postoperative explosive pain in patients with femoral neck fracture[J]. Chinese Journal of General Practice, 2022, 20(9): 1498-1501. doi: 10.16766/j.cnki.issn.1674-4152.002633 [3] XU B Y, YAN S, LOW L L, et al. Predictors of poor functional outcomes and mortality in patients with hip fracture: a systematic review[J]. BMC Musculoskelet Disord, 2019, 20(1): 568. doi: 10.1186/s12891-019-2950-0 [4] SHEEHAN K J, GUERRERO E M, TAINTER D, et al. Prognostic factors of in-hospital complications after hip fracture surgery: a scoping review[J]. Osteoporos Int, 2019, 30(7): 1339-1351. doi: 10.1007/s00198-019-04976-x [5] SHEEHAN K J, WILLIAMSON L, ALEXANDER J, et al. Prognostic factors of functional outcome after hip fracture surgery: a systematic review[J]. Age Ageing, 2018, 47(5): 661-670. doi: 10.1093/ageing/afy057 [6] VOLKERT D, BECK A M, CEDERHOLM T, et al. ESPEN guideline on clinical nutrition and hydration in geriatrics[J]. Clin Nutr, 2019, 38(1): 10-47. doi: 10.1016/j.clnu.2018.05.024 [7] 中华医学会骨科学分会创伤骨科学组, 中国医师协会骨科医师分会创伤专家工作委员会. 成人股骨颈骨折诊治指南[J]. 中华创伤骨科杂志, 2018, 20(11): 921-928. doi: 10.3760/cma.j.issn.1671-7600.2018.11.001Department of Traumatic Osteology, Orthopedic Branch of Chinese Medical Association, Working Committee of Trauma Experts, Orthopedic Branch of Chinese Medical Association. Guidelines for diagnosis and treatment of adult femoral neck fractures[J]. Chinese Journal of Orthopaedic Trauma, 2018, 20(11): 921-928. doi: 10.3760/cma.j.issn.1671-7600.2018.11.001 [8] BUDZYNSKI J, TOJEK K, CZERNIAK B, et al. Scores of nutritional risk and parameters of nutritional status assessment as predictors of in-hospital mortality and readmissions in the general hospital population[J]. Clin Nutr, 2016, 35(6): 1464-1471. doi: 10.1016/j.clnu.2016.03.025 [9] VERONESE N, VIANELLO S, DANESIN C, et al. Multidimensional prognostic index and mortality in intermediate care facilities: a retrospective study[J]. J Clin Med, 2021, 10(12): 2632. doi: 10.3390/jcm10122632 [10] KHAJURIA A, KRAHN J. Osmolality revisited: deriving and validating the best formula for calculated osmolality[J]. Clin Biochem, 2005, 38(6): 514-519. doi: 10.1016/j.clinbiochem.2005.03.001 [11] SABANOVIC K, SKJØDE DAMSGAARD E M, GREGERSEN M. Preoperative dehydration identified by serum calculated osmolarity is associated with severe frailty in patients with hip fracture[J]. Clin Nutr Espen, 2022, 52: 94-99. doi: 10.1016/j.clnesp.2022.10.006 [12] MCCROW J, MORTON M, TRAVERS C, et al. Associations between dehydration, cognitive impairment, and frailty in older hospitalized patients: an exploratory study[J]. J Gerontol Nurs, 2016, 42(5): 19-27. doi: 10.3928/00989134-20160201-01 [13] EKMAN L, JOHNSON P, HAHN R G. Signs of dehydration after hip fracture surgery: an observational descriptive study[J]. Medicina(Kaunas), 2020, 56(7): 361. [14] ZANETTI M, DE COLLE P, OMICIUOLO C, et al. Postoperative dehydration is associated with frailty and decreased survival in older patients with hip fracture[J]. Nutrients, 2022, 14(4): 820. doi: 10.3390/nu14040820 [15] BERSKA J, BUGAJSKA J, SZTEFKO K. The accuracy of serum osmolarity calculation in small children[J]. J Med Biochem, 2023, 42(1): 67-77. doi: 10.5937/jomb0-37490 [16] LORENTE J V, REGUANT F, ARNAU A, et al. Effect of goal-directed haemodynamic therapy guided by non-invasive monitoring on perioperative complications in elderly hip fracture patients within an enhanced recovery pathway[J]. Perioper med (Lond), 2022, 11(1): 46. doi: 10.1186/s13741-022-00277-w [17] KUSEN J Q, SCHAFROTH B, POBLETE B, et al. The implementation of a Geriatric Fracture Centre for hip fractures to reduce mortality and morbidity: an observational study[J]. Arch Orthop Trauma Surg, 2019, 139(12): 1705-1712. doi: 10.1007/s00402-019-03229-0 [18] KUSEN J Q, VAN DER VET P, WIJDICKS F, et al. Does preoperative hemodynamic preconditioning improve morbidity and mortality after traumatic hip fracture in geriatric patients? A retrospective cohort study[J]. Arch Orthop Trauma Surg, 2021, 141(9): 1491-1497. [19] YAN B, SUN W, WANG W, et al. Prognostic significance of frailty in older patients with hip fracture: a systematic review and meta-analysis[J]. Int Orthop, 2022, 46(12): 2939-2952. doi: 10.1007/s00264-022-05605-9 [20] ZHAO H, WEI P, FENG Y. Association between frailty and clinical outcomes and quality of life in older adults following hip fracture surgery: a retrospective cohort study[J]. Anesth Analg, 2022, 134(5): 1035-1042. doi: 10.1213/ANE.0000000000005841 [21] ZANETTI M, MARZARO G, DE COLLE P, et al. Predictors of short- and long-term mortality among acutely admitted older patients: role of inflammation and frailty[J]. Aging Clin Exp Res, 2022, 34(2): 409-418. doi: 10.1007/s40520-021-01926-8 [22] WILLIS J, PELZL C E, JARVIS S, et al. Significant variations in preoperative fluid resuscitation volumes delivered to elderly hip fracture patients at six level 1 trauma centers: an observational descriptive study[J]. OTA Int, 2022, 5(1): e162. DOI: 10.1097/OI9.0000000000000162. -





 下载:
下载: