Analysis of the efficacy of combined immunotherapy and radiotherapy in patients with brain metastasis from driver-gene negative non-small cell lung cancer
-
摘要:
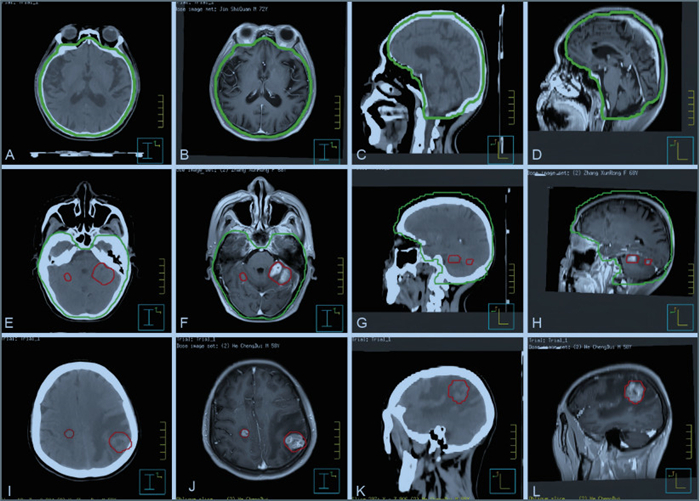
目的 探讨免疫治疗联合颅脑放疗对驱动基因阴性非小细胞肺癌(NSCLC)脑转移患者的疗效和安全性。 方法 选择2020年1月—2023年12月蚌埠医科大学第一附属医院收治的108例NSCLC脑转移患者作为研究对象。根据治疗方法将患者分为单纯颅脑放疗组(单一组,60例)和免疫联合颅脑放疗组(联合组,48例),比较单一组和联合组的疗效和毒副作用。此外,将联合组患者根据颅脑放疗模式的不同进一步分为A组[全脑放疗(WBRT)]、B组(WBRT联合局部加量放疗)和C组(局部放疗)3个亚组,比较3组不同放疗模式的治疗效果和副作用。 结果 联合组的颅内客观有效率(iORR)和颅内疾病控制率(iDCR)均高于单一组[54.17%(26/48) vs. 35.00%(21/60),χ2=3.985, P=0.046;75.00%(36/48) vs. 56.67%(34/60),χ2=3.930, P=0.047],治疗期间2组的不良反应均可耐受。联合组各亚组颅内疗效比较显示B组的iORR和iDCR均高于A组(P < 0.001),毒副作用发生率在3组间差异无统计学意义(P>0.05)。 结论 免疫治疗联合颅脑放射治疗对驱动基因阴性NSCLC脑转移患者安全有效,提高颅内疾病控制率的同时不增加毒副作用。 Abstract:Objective Exploring the efficacy and safety of combined immunotherapy and radiotherapy in patients with brain metastasis from driver-gene negative non-small cell lung cancer (NSCLC). Methods A total of 108 NSCLC patients with brain metastasis, admitted to the First Affiliated Hospital of Bengbu Medical University from January 2020 to December 2023, were selected as the research objects. Patients were divided into the cranial radiotherapy group (single group, 60 cases) and the combined immunotherapy plus cranial radiotherapy group (combined group, 48 cases) according to treatment Methods. The efficacy and toxicity of the two groups were compared. In addition, patients in the combined therapy group were further subdivided into three subgroups: group A (whole brain radiotherapy, WBRT), group B (WBRT combined with local dose radiotherapy), and group C (local radiotherapy) according to the different modes of cranial radiotherapy. The treatment outcomes and side effects of the different radiotherapy modes were compared among the subgroups. Results The intracranial Objective response rate (iORR) and disease control rate (iDCR) in the combined therapy group were higher than those of the single therapy group [54.17% (26/48) vs. 35.00% (21/60), χ2=3.985, P=0.046; 75.00% (36/48) vs. 56.67% (34/60), χ2=3.930, P=0.047]. Both groups had tolerable adverse reactions. The comparison of intracranial efficacy among the three subgroups in the combined therapy group showed that the iORR and iDCR of group B were higher than those in the group A (P < 0.001), with no significant difference in the incidence of side effects among the three groups (P>0.05). Conclusion Immunotherapy combined with radiotherapy is effective in patients with brain metastasis from driver gene-negative NSCLC. This combination improves the disease control rate without significantly increasing side effects. -
Key words:
- Non-small cell lung cancer /
- Brain metastasis /
- Driver gene negative /
- Immunotherapy /
- Radiation therapy
-
表 1 2组NSCLC脑转移患者临床资料比较[例(%)]
Table 1. Comparison of clinical data between two patient groups with brain metastases in NSCLC[cases(%)]
项目 单一组
(n=60)联合组
(n=48)χ2值 P值 性别 0.140 0.708 男性 47(78.33) 39(81.25) 女性 13(21.67) 9(18.75) 年龄(岁) 0.438 0.508 < 60 25(41.67) 17(35.42) ≥60 35(58.33) 31(64.58) BMI 0.270 0.603 < 24 32(53.33) 28(58.33) ≥24 28(46.67) 20(41.67) 吸烟史 0.121 0.728 有 33(55.00) 28(58.33) 无 27(45.00) 20(41.67) 治疗线数 3.590 0.058 1 36(60.00) 20(41.67) ≥2 24(40.00) 28(58.33) 病理类型 3.510 0.061 腺癌 39(65.00) 39(81.25) 非腺癌 21(35.00) 9(18.75) 脑转移瘤数目 2.645 0.104 1~3 32(53.33) 33(68.75) >3 28(46.67) 15(31.25) 表 2 2组NSCLC脑转移患者颅内疗效比较[例(%)]
Table 2. Comparison of intracranial efficacy between two patient groups with brain metastases in NSCLC[cases(%)]
组别 例数 CR PR SD PD iORR iDCR 单一组 60 0 21(35.00) 13(21.67) 26(43.33) 21(35.00) 34(56.67) 联合组 48 2(4.17) 24(50.00) 10(20.83) 12(25.00) 26(54.17) 36(75.00) χ2值 3.985 3.930 P值 0.046 0.047 表 3 2组NSCLC脑转移患者毒副作用比较[例(%)]
Table 3. Comparison of toxic and side effects between two patient groups with brain metastases in NSCLC[cases(%)]
组别 例数 白细胞计数下降 放射性脑损伤 免疫相关性肺炎 反应性毛细血管增生症 单一组 60 17(28.33) 2(3.33) 0 0 联合组 48 12(25.00) 2(4.17) 2(4.17) 23(47.92) χ2值 0.151 36.529 P值 0.698 0.999a 0.195a < 0.001 注:a为使用Fisher精确检验。 表 4 不同放疗模式亚组NSCLC脑转移患者颅内疗效比较[例(%)]
Table 4. Comparison of intracranial efficacy across subgroups with different radiotherapy modalitie[cases(%)]
组别 例数 CR PR SD PD iORR iDCR A组 13 0 3(23.08) 3(23.08) 7(53.85) 3(23.08) 6(46.15) B组 14 1(7.14) 9(64.29) 3(21.43) 1(7.14) 10(71.43)a 13(92.86)a C组 21 1(4.76) 12(57.14) 4(19.05) 4(19.05) 13(61.90) 17(80.95) χ2值 7.248 7.661 P值 0.027 0.018 注:与A组比较,aP < 0.017。 表 5 不同放疗模式亚组NSCLC脑转移患者毒副作用比较[例(%)]
Table 5. Comparison of toxicity and side effects across subgroups with different radiotherapy modes[cases(%)]
组别 例数 白细胞计数下降 放射性脑损伤 免疫相关性肺炎 反应性毛细血管增生症 A组 13 4(30.77) 0 1(7.69) 8(61.5) B组 14 5(35.71) 1(7.14) 1(7.14) 6(42.9) C组 21 3(14.29) 1(47.62) 0 9(42.9) χ2值 1.326 P值 0.326a 0.999a 0.311a 0.515 注:a为采用Fisher精确检验。 -
[1] SIEGEL R L, GIAQUINTO A N, JEMAL A. Cancer statistics, 2024[J]. CA Cancer J Clin, 2024, 74(1): 12-49. doi: 10.3322/caac.21820 [2] 郑荣寿, 陈茹, 韩冰峰, 等. 2022年中国恶性肿瘤流行情况分析[J]. 中华肿瘤杂志, 2024, 46(3): 221-231. doi: 10.3760/cma.j.cn112152-20240119-00035ZHENG R S, CHEN R, HAN B F, et al. Prevalence of malignant tumors in China in 2022[J]. Chinese Journal of Oncology, 2024, 46(3): 221-231. doi: 10.3760/cma.j.cn112152-20240119-00035 [3] LAMBA N, KEARNEY R B, CATALANO P J, et al. Population-based estimates of survival among elderly patients with brain metastases[J]. Neuro Oncol, 2021, 23(4): 661-676. doi: 10.1093/neuonc/noaa233 [4] HENDRIKS L E, KERR K M, MENIS J, et al. Oncogene-addicted metastatic non-small-cell lung cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up[J]. Ann Oncol, 2023, 34(4): 339-357. doi: 10.1016/j.annonc.2022.12.009 [5] HENDRIKS L E, KERR K M, MENIS J, et al. Non-oncogene-addicted metastatic non-small-cell lung cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up[J]. Ann Oncol, 2023, 34(4): 358-376. doi: 10.1016/j.annonc.2022.12.013 [6] ALTAN M, WANG Y, SONG J, et al. Nivolumab and ipilimumab with concurrent stereotactic radiosurgery for intracranial metastases from non-small cell lung cancer: analysis of the safety cohort for non-randomized, open-label, phase Ⅰ/Ⅱ trial[J]. J Immunother Cancer, 2023, 11(7): e6871. DOI: 10.1136/jitc-2023-006871. [7] 陈旭澜, 李泞甫, 肖剑波, 等. 非小细胞肺癌脑转移的免疫治疗现状及进展[J]. 中国临床研究, 2023, 36(6): 821-826.CHEN X L, LI N F, XIAO J B, et al. Current status and progress of immunotherapy for brain metastases in non-small cell lung cancer[J]. Chinese Journal of Clinical Research, 2023, 36(6): 821-826. [8] 孙逸初, 梁飞, 夏铀铀. 非小细胞肺癌脑转移放疗联合免疫治疗的研究进展[J]. 肿瘤防治研究, 2023, 50(7): 705-709. doi: 10.3971/j.issn.1000-8578.2023.22.1322SUN Y C, LIANG F, XIA Y Y. Research progress on brain metastases combined with radiotherapy combined with immunotherapy for brain metastases in non-small cell lung cancer[J]. Cancer Prevention and Treatment Research, 2023, 50(7): 705-709. doi: 10.3971/j.issn.1000-8578.2023.22.1322 [9] CASTELLANI G, CROESE T, PERALTA RAMOS J M, et al. Transforming the understanding of brain immunity[J]. Science, 2023, 380(6640): eabo7649. DOI: 10.1126/science.abo7649. [10] LI M, HOU X, SAI K, et al. Immune suppressive microenvironment in brain metastatic non-small cell lung cancer: comprehensive immune microenvironment profiling of brain metastases versus paired primary lung tumors (GASTO 1060)[J]. OncoImmunology, 2022, 11(1): 2059874. DOI: 10.1080/2162402X.2022.2059874. [11] WANG Y, WANG L, LI T, et al. Bimetallic nanoparticles as cascade sensitizing amplifiers for low-dose and robust cancer radio-immunotherapy[J]. Acta pharmaceutica Sinica. B, 2024, 14(4): 1787-1800. doi: 10.1016/j.apsb.2023.11.028 [12] MANSFIELD A S, HERBST R S, DE CASTRO G J, et al. Outcomes with pembrolizumab monotherapy in patients with programmed death-ligand 1-positive NSCLC with brain metastases: pooled analysis of KEYNOTE-001, 010, 024, and 042[J]. JTO Clin Res Rep, 2021, 2(8): 100205. DOI: 10.1016/j.jtocrr.2021.100205. [13] 郑晓丽, 王晓辉, 孙亚楠, 等. 非小细胞肺癌脑转移一线免疫联合放疗疗效分析[J]. 中华放射肿瘤学杂志, 2023, 32(12): 1044-1050. doi: 10.3760/cma.j.cn113030-20221009-00333ZHEGN X L, WANG X H, SUN Y N, et al. Efficacy of first-line immunotherapy combined with radiotherapy for brain metastases in non-small cell lung cancer[J]. Chinese Journal of Radiation Oncology, 2023, 32(12): 1044-1050. doi: 10.3760/cma.j.cn113030-20221009-00333 [14] ABDULHALEEM M, JOHNSTON H, D' AGOSTINO R J R, et al. Local control outcomes for combination of stereotactic radiosurgery and immunotherapy for non-small cell lung cancer brain metastases[J]. J Neurooncol, 2022, 157(1): 101-107. doi: 10.1007/s11060-022-03951-7 [15] PORTE J, SAINT-MARTIM C, FREDERIC-MOREAU T, et al. Efficacy and safety of combined brain stereotactic radiotherapy and immune checkpoint inhibitors in non-small-cell lung cancer with brain metastases[J]. Biomedicines, 2022, 10(9): 2249. DOI: 10.3390/biomedicines10092249. [16] VELLAYAPPAN B A, MCGRANAHAN T, GRABER J, et al. Radiation necrosis from stereotactic radiosurgery: How do we mitigate?[J]. Curr Treat Options Oncol, 2021, 22(7): 57. DOI: 10.1007/s11864-021-00854-z. [17] LEHRER E J, AHUWALIA M S, GUREWITZ J, et al. Imaging-defined necrosis after treatment with single-fraction stereotactic radiosurgery and immune checkpoint inhibitors and its potential association with improved outcomes in patients with brain metastases: an international multicenter study of 697 patients[J]. J Neurosurg, 2022, 138(5): 1178-1187. [18] ZHU K K, WEI J L, XU Y H, et al. Effect of stereotactic body radiation therapy on diverse organ lesions in advanced non-small cell lung cancer patients receiving immune checkpoint inhibitors[J]. Curr Med Sci, 2023, 43(2): 344-359. doi: 10.1007/s11596-023-2702-0 [19] 董晶. 肺癌脑转移患者全脑放疗后认知功能状况的研究[J]. 中华放射肿瘤学杂志, 2023, 32(10): 900-906. doi: 10.3760/cma.j.cn113030-20230203-00020DONG J. Study on cognitive function of patients with brain metastases of lung cancer after whole-brain radiotherapy[J]. Chinese Journal of Radiation Oncology, 2023, 32(10): 900-906. doi: 10.3760/cma.j.cn113030-20230203-00020 [20] 赵皓, 齐学远, 王俊斌, 等. 外周血淋巴细胞亚群在非小细胞肺癌中的表达及意义[J]. 中华全科医学, 2023, 21(11): 1849-1851.ZHAO H, QI X Y, WANG J B, et al. Expression and significance of peripheral blood lymphocyte subsets in non-small cell lung cancer[J]. Chinese Journal of General Practice, 2023, 21(11): 1849-1851. [21] 王朝, 韩雪, 张爱霞. LIPI评分对PD-1/PD-L1抑制剂治疗非小细胞肺癌效果与预后的价值分析[J]. 中国现代医学杂志, 2023, 33(6): 55-60.WANG C, HAN X, ZHAGN A X. Value analysis of LIPI score on the efficacy and prognosis of PD-1/PD-L1 inhibitors in the treatment of non-small cell lung cancer[J]. Chinese Journal of Modern Medicine, 2023, 33(6): 55-60. -





 下载:
下载: